Implant Placed Very Close to Adjacent Tooth and Buccal Wall Disintegrating: Should I Open the Flap?
Dr. S. asks:
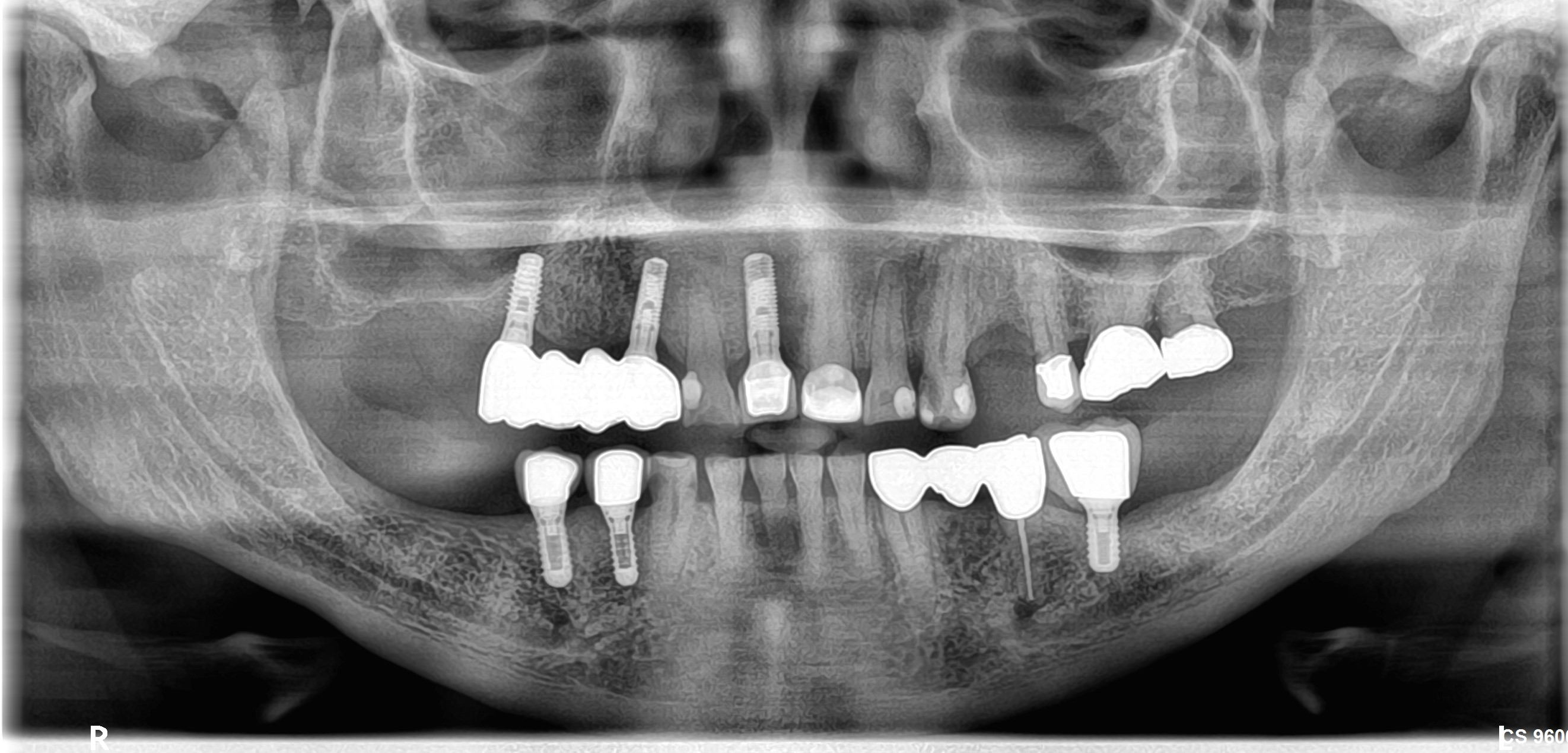
I am a periodontist. I had placed an implant in #5 position [maxillary right first premolar; 14]. #4 [maxillary left first premolar; 15] had been extracted 3 weeks prior. I placed the implant very close to #6 [maxillary right canine ; 13]. The patient returned at 2 weeks post-operative and presented with a fluctuant swelling in the mucobuccal fold and a periapical radiolucent lesion around the implant and canine. Purulent drainage from the swelling was copious. I initiated root canal treatment in #6 and prescribed antibiotics. The buccal wall over the implant appeared to be disintegrating although the implant appeared to be osseointegrating. What should I do at this point? Do I open the flap?

16 Comments on Implant Placed Very Close to Adjacent Tooth and Buccal Wall Disintegrating: Should I Open the Flap?
New comments are currently closed for this post.
mike ainsworth
7/11/2011
oops, sorry my friend, but i think this one is a gonner. Just have to take it on the chin, endo the tooth, wait and pop another back in. sorry.
Guy Carnazza
7/11/2011
It is very early in the game so best option would be to open area, remove implant, reposition and graft. Perform vitality tests on the #6. If needed perform endo .
Dr. Dan
7/12/2011
Take out the implant, graft the area, let it heal. Make sure the root canal is good and redo the implant.
david
7/12/2011
remove loose implant, regraft and evaluate vitality of 6 as possible source of infection.
Dr. Martin
7/12/2011
No question about it, ex-implantation #5 and wait 6-8 weeks, new implant. Maybe an idea implantation regio 4 and then bridge cantilever, if extensive buccal bone loss regio 5. Implantation regi 5 and 12, always necessary with a lots of attention to root of the canine. Recommend peroperatve xray
Dr. Wolanski
7/12/2011
I agree with the comments to remove the implant yesterday. Aggresively treat the infection and you may prevent loosing the crestal bone which will be much harder to replace that the apical bone (even if it fenestrates)
Jon
7/12/2011
You state you are a periodontist but you performed RCT on #6 yourself? I did not know periodontists did endo. I am a periodontist and am surprised you would not know how to treat the area. Definitely remove the implant (I have not seen the patient clinically but radiographically the implant with all of the apical and surrounding bone loss I highly doubt the implant is integrating as you state it is) as it is only going to get worse leaving it in place and wasting time. Also, does the "buccal wall" you refer to mean the buccal plate or are you talking about losing the bone interproximal of 5-6? I suspect you mean the IP of 5-6 area as this bone, if the implant is not removed, may necrose and you will have a really big problem on your hands then and may lose #6 as well if the bone does not "regenerate" but granulation tissue is allowed to form. Since you started endo on #6 you need to complete it or have someone do so (does perio really do endo?). You need to remove the implant ASAP and degranulate area to bone. Have pt. on antibiotics for a few days prior to this and 7-10 days afterwards. I would try a bone graft (particulate bone most likely depending on what the defect looks like at the time of flap reflection as I think a block graft in an actively infected site is more likely not to heal well) to at least try to attempt to prevent more collapse of the soft tissue but would let the pt. know that more bone grafting prior to implant may still be necessary (such as block grafting depending on how much bone you lose). Looking at the radiograph I just hope you still have some buccal and lingual plate left and both are not destroyed through and through. Try to bulk the area out as much as possible with primary closure and a membrane and a tension free flap because you most likely will get a fair amount of ridge collapse anyway with this case. There is also risk of graft infection when you place the graft and remove the implant at the same time so be diligent in removing the infected granulation tissue to bone well and thorough irrigation and debridemen. I would also mix the graft with antibiotic as well. Once bone has healed replace implant but watch angulation (again second bone graft may be needed just looking radiographically at the photo without clinical views). I am still suspicious you are really a periodontist but I wish you luck regardless. I would hope a non specialist would not post posing as a specialist as it gives the specialist in that discipline a bad name and makes all in our specially look incompetent. Also, inform the pt. ASAP of what is going on (hopefully you have at least had them sign previously a consent form but this will not mean much in court regardless) and I would do the RCT, and any bone graft at no charge (possibly even the implant or at cost) and pray you are not sued. If you are not a periodontist or are not comfortable with this refer to another periodontist ASAP to treat. If you are a periodontist, please make sure to go to some CE courses on implants, bone grafting, implant complications, etc. My goal is not to be mean or to come off sounding mean (please do not take it that way as it is not meant to be) I am really just very perplexed with the situation and question for a specialist to ask in this clear cut situation on removing the implant or not. Good luck.
Dr.B
7/12/2011
I am a periodontist as well and I think I couldn't have stated it better than Jon above. I agree with his recommendation. With all due respect to the author ofcourse.
Dr Ares
7/14/2011
Dr S.,
The site had copious purulent drainage, and it has obvious radiografic signs of infection, so, I don't agree with your opinion that this implant is osseointegrating. Remove the offending implant soon, wait for healing and place new implant and graft if neccessary!
Hope all goes well.
PCPerio
7/14/2011
These are all good clinical suggestions but I would definitely not graft at the time of implant removal. Too many things can go wrong. Let the site heal after removing the implant then plan your next move.
Where I disagree is the endo part. As a periodontist you are an expert in many aspects of clinical dentistry. Endo is not one of them. We always encourage clinicians to practice within their scope of expertise and I think you should follow that approach. Remove the implant and get an endo consult.
Hope all goes well.
PC
TOBooth BDS Hons MSc (OMF
7/15/2011
Defo,
never never graft an infected site chaps!!!!!
Ever!
ttmillerjr
7/16/2011
Bolonga TOBooth, but in this case I agree not to graft at explantation.
Richard Hughes, DDS, FAAI
7/16/2011
Remove the implant, degranulate, detoxify and irrigate the site. Reimplant at a later date (after healing)and angle the implant to the distal to avoid the cuspid. Obtain an endo consult. You may have to graft the site prior to implantation.
Francois
7/17/2011
May I speak about the your future surgeries?
We should always take an x-ray of the the first drill to confirm position and angulation.
Also the flap should expose the root convexity of the cuspid. It is usually quite visible and will help keeping the proper angulation.
A final x-ray of the implant in place is always done at the end of the surgery. That is the proper time to decide that the result is not as we would want it, remove the implant, tell the patient whatever will make everybody happy and show how much you care and how meticulous you are.
Then redo implant later.
Would you have left this implant in your mouth? your spouse's mouth?
We all have to be prepared to react properly when seeing the final x-ray as it is normal that it sometimes shows poor result. Happens to everyone.
regards.
Greg Steiner
7/18/2011
The implant needs to be removed of course. I suggest you remove the granulation tissue and if there is any area where the root of #6 was damaged that needs to be smoothed otherwise it will contain bacteria that will prevent healing. Leaving the area open will result in colonization of the root surface by oral bacteria. Treat it like any other periodontal lesion and you should be fine. Graft the site with a graft material that does not have macropores to reduce the potential for bacterial colonization of the graft material. As a periodontist doing nothing but regenerative therapy I graft infected extraction sites and periodontal lesions ever every day I work and I cannot remember the last time I have had a post operative infection or infected graft site. I have been doing implants for 28 years and if you feel like it would be beneficial we have dentists visiting the Bone Institute to view our procedures and there is no charge. Greg Steiner Steiner Laboratories
Fabio B
7/28/2011
The implant in 14 (#5) is really too close to 13 and clearly infected. Remove and clean accurately. Keep attention for vitality of canine, the teeth could be necrotic. Insert a new implant after 6-8 weeks.