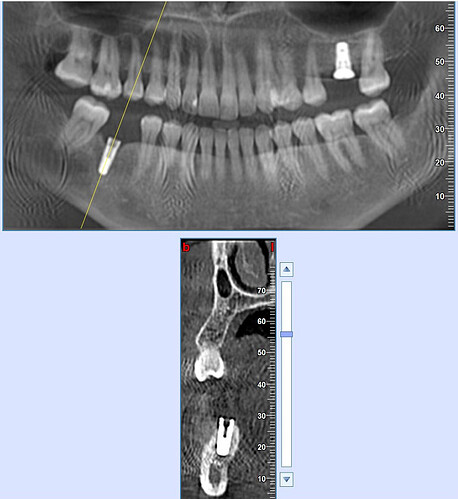
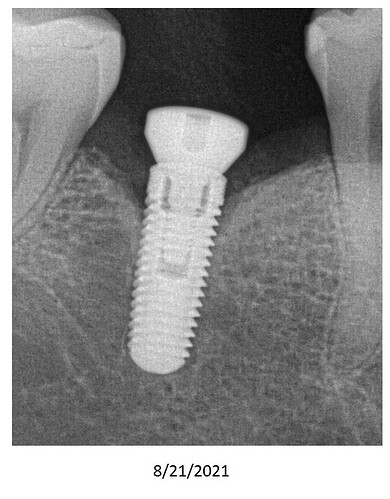
I have a patient with a poorly placed internal hex implant fixture. The head of the implant has become exposed through the gingiva, along with crestal bone loss. Images of this have been uploaded below. I am considering the removal of the implant, grafting, and replacement. In the alternative, a 3-unit tooth supported bridge is also considered. How would you approach the treatment for this case? Insight from other clinicians is greatly appreciated - thank you!
Roger Gomez comments:
If the implant is stable and the soft tissues are OK, it all depends on how confident you are on producing a vertical improvement or getting a second opinion from a Periodontist. A Periodontist will greatly help in the decision making. Just remember that those implant cases might be a nightmare so the most important issue for me is the communication with the patient...at least it has been my experience, Good Luck !!!Jun Carlos Flores (perio) comments:
Extract the implant. The platform seems not deep enough, so, the emergence contour will no be the ideal compromising the plaque control. This, in addition to the exposed threads will be a receipt for failure.Peter Hunt comments:
This is a tricky case. At this stage, the implant is obviously well integrated which will make it difficult to remove.There has been recession of the labial bone, which as we all know is common post-extraction. The alveolus is narrow and there is no room to position a replacement implant more to the lingual.The best way to approach the situation is to create a “window” out to the labial of the implant preferably with a piezo saw tip. The implant can then be tipped out to the labial, leaving a partially intact socket which can be deepened or expanded to receive a new implant. This should be shorter in length than the current implant, so that the platform of the implant is 3-4mm below the crest of the bone.The labial plate in the region should be perforated extensively through the cortical bone and augmented with a suitable bone graft and covered with a membrane.
Allow the region to settle and heal 3-4 months before considering final restoration.
Timothy Carter comments:
Assuming this is a stable well integrated implant then it is only a pride issue. It has some loss to the 2nd/3rd thread and per your description soft tissue recession on the labial… so what. I have treated these cases successfully for 15+ with soft tissue augmentation, either connective tissue or free gingival graft, purely for the purpose of increasing the band of KG and protecting the supporting bone. It may have some gray at the margin but it is a lower posterior and if you have thick connective tissue with adequate hygiene it will be fine. Sorry for the disappointment but it does not need removal and bone grafting with fancy products just a good old fashion soft tissue graft and a tooth on topA J comments:
I agree with ya! If patient's doing OK, should just leave it alone. If needs to be replaced? why do it now or wait.......... could wait and do it later (years from now that is)?? I've seen cases where unattractive implants still there 10 years later.Gerald M. Marlin, DMD, MS comments:
Since it appears that the head of the implant is approximating the height of the mesial and distal bone, I would take a CBCT to evaluate the defect. If it is a circumferential one having a 3 wall infrabony pocket, which is frequently the case, I would replace the healing abutment with a cover screw after reflecting the tissue and curette the complete defect until completely clean. I would then detoxify the implant and place .5cc of cancellous bone with a growth factor and suture the site closed over a Biomen Xtend or equivalent long term, resorbable barrier membrane. I have many cases where the implant has been salvaged. In the event that this does not work, I would remove the implant and regraft the site-*without any implant placement *until full bone integration.Guest comments:
Restoring an already failing implant is probably not wise. If that CBCT film was an intraoperative film it was placed too shallow at the get go. Was a surgical guide used to correlate with the cbct?A J comments:
If patient's not in pain and the tooth's functioning fine? However, probably doesn't look cosmetically pleasing in the non-esthetic zone ( anterior v posterior ) with metal partly exposed? Why lose sleep over it? You go over it ( the issues or not) with the patient. With the patient's understanding, the recommendation is to recall every 6 months for follow up?Dr Pravin Patel comments:
Looks like a case of cover screw abscess..once gingival former is placed , should heal and bone is formed, whatever is currete the defect , place bone graft and place healing abutment again, whatever the results definitely restore it, it has a enough life without complications in most of the cases..soft tissue grafting only if thin gingival biotype and buccaly exposed which may leads to more open thread in future..but surely should restore...all the bestMahijeet Singh Puri comments:
It seems from your scan that you placed a bigger Dia implant which is the cause of your problem. There is definitely v shaped bone loss around the implant. How much time has passed since the implant has been placed. If implant is well osseointegrated Do the treatment of peri implantitis as recommended.