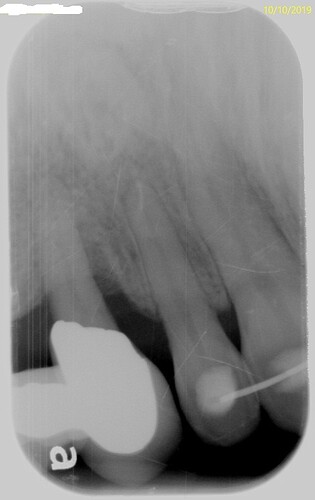
The following case initially presented to me 2 years ago with a 4-6 FPD and ailing #6 abutment. Initially I tried to preserve #6 through conventional periodontal treatment and placed a single implant with immediate provisional #5. After nearly 1.5 years the patient decided to have #6 removed and I did not feel it was a good candidate for an implant as the risk of further esthetic compromise was high. Treatment consisted of removing the provisional #5 and extracting #6. The extraction site was grafted with porcine xenograft (Salvin Oss, Salvin Dental) and a pedicle connective tissue graft was rotated from the palate to cover the graft and augment the facial and closed with 4-0 chromic gut suture. A new screw retained bis-acryl provisional was fabricated (Provisa Plus, Benco Dental) with an ovate cantilever pontic and allowed to blanch the tissue in an effort to sculpt and shape the pontic site. The patient is expected to be in this provisional for at least 8-12 weeks and at approximately 4 weeks it will be removed and modified PRN.


DrT comments:
By retaining #6 when you placed implant in #5 you compromised the bone in the mesial of the implant..I would have removed #6 at the same time as I inserted implant in #5
Timothy Carter comments:
I agree but the patient wanted to keep 6 if possible and I really hate for patients to lose a canine. I am confident that by using an ovate pontic and thick connective tissue that there will be soft tissue papilla fill but it wont happen over night. I believe there are numerous different ways to handle this case but IMHO the only wrong approach would be treating it as a case of titanium deficiency and placing 2 fixtures. The final photo is only 2 weeks post treatment and the soft tissue is far from mature. Also that provisional is attached to the fixture mount of a Zimmer TSV so a final restoration will have less metal to show.
Jpk comments:
A let’s go Brandon treatment plan !
Pros doc comments:
Cantilevering a highly functional tooth like a cupid has a poor long term prognosis. You've allowed the patient yo dictate treatment. You have good bone height to Mesilla or #4 and distal of #7 so remove the cupid and implant, graft the entire span, then two implants. Or, the anterior font look stellar so maybe get them out and create an implant supported FPD? Then the cupid could be a poetic. But cantilevering a cupid, in my opinion, is never an option
Timothy Carter comments:
I agree but this patient had lost her cuspid guidance long ago... not much function on the so called canine she had. You make a good point that I let the patient dictate treatment but I never lose any sleep over letting hard working American citizens decide for themselves what they want... Lets Go Brandon!!!
User comments:
you just lost me with "Lets go Brandon"!
Timothy Carter comments:
One reason I put this up here is because this case defies a lot of conventional wisdom such as cantilever a canine which is a general no no. In her case she had been functioning on a compromised canine devoid of guidance so that canine was essentially a glorified incisor. An implant in the canine site could reduce the papilla height on the distal of the lateral and an ovate pontic can predictably yield about 2.5mm additional soft tissue height. so I do not pretend that my treatment is ideal but it is what the patient was comfortable with. I can only speak for myself but if I allow my ego to get in the way in the area of the country I practice then my dental career will be quite short.
Perio Doc comments:
Its easy to let a patient steer our treatment planning and I understand that. However if you consistently provide what you know is sound treatment that works well and lasts, your community reputation will do nothing but improve. I would have treated this case by extraction of #6 with grafting of the #5 and #6 sites using an allograft with a good barrier membrane. 6 months later I would place two implants.
Hedieh comments:
I am a simple by-stander, and would like to know if it is good practice to place an implant next to a tooth that is periodontally compromised and is a great area for bacteria to linger? Is it best to remove that tooth, at the same time the implant was placed? I have cantilevered two premolar crowns on one implant without any issues, but I am very curious to see how this turns out. I understand when patients may not have the funds for what we would prefer to do, and sometimes you have to compromise and take good in place of perfect.
Timothy Carter comments:
I really appreciate all of the responses on this. I am preparing cases to present to residents and I like to get some feedback from others docs for good discussion. Thanks again and I apologize for the Let’s Go Brandon as it intended to reference the independent minded nature of the patient.