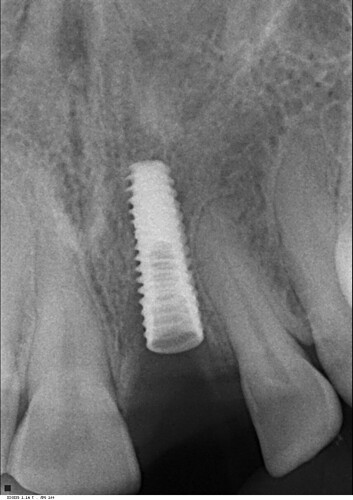
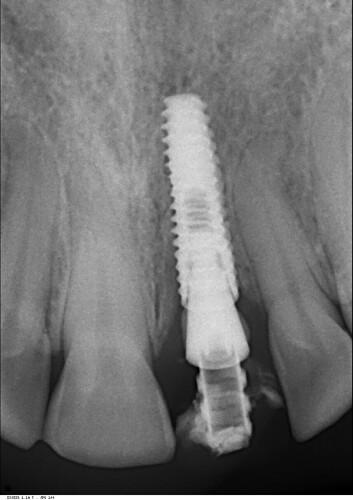
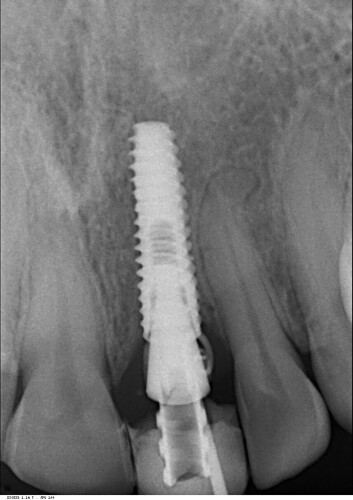
I did this immediate implant 3 months back. Labial cortex was damaged coronally, but apically was good. So we placed an immediate implant after atraumatic extraction and gave a temporary crown. 2 months later the patient presented with an abscess with a sinus. Radiograph was good at that time with no unexpected bone loss. So we prescribed her antibiotics and it resolved within a week. Now again after 1 month she came with a sinus complication. Attaching present radiographic images also. This time we removed the temporary crown. The gingiva was slightly inflamed. We put a healing abutment this time after thorough irrigation. The temporary crown, on careful observation was slightly rough at one area. We are thinking that this must be the reason for the microbial plaque accumulation and subsequent pericoronitis. Please provide your expert opinion and comments for this. We are still learning and appreciate your help. How should we proceed now?
Dr KG comments:
Immediate placement is always high risk. Especially if you had a necrotic or infectious tooth. My advice: untorque and remove the implant. Let it heal for 6-8 weeks. Implant afresh.Dr KG comments:
Further, by now you have a buccal perforation(grafting needed), and 2.2 might be necrotic as well requiring RCT.STW comments:
2.2 doesn't look necrotic? Where you see that?Dr KG comments:
I said MIGHT be necrotic. Widened PDL, apical area? worth doing a vit testSM52 comments:
I doubt #22 is infected, there is no reason it would be. Immediate implant placement is not high risk if done in the right sights by someone who is good or has experience.This implant though is a problem and removal and a new implant is the most predictable approach. Determine at the removal whether socket augmentation is needed, then place the next implant with the bone/gingiva is ready.
dsdds comments:
Seeing the dark shadow along the soft tissue. the implant may have been place labially. Do you have a 3d xray?NPDMD comments:
Take a CBCT. You may not have any facial bone, which would lead to the draining labial infection. If that's the case, implant removal and grafting would be indicated.otis scud comments:
these are tricky cases... old broken endo in esthetic zone with some crestal bone loss, even with an atraumatic extraction , then an immediate implant and immediate temp. I always let these cases heal before I implant. Here is what I do, i make a flipper because I expect the thin and in this case missing crestal portion of buccal bone must be dealt with at the time of extraction. After extraction of an endo tooth, expect the apex to have pathogens, take a long 702 bur, not a spoon, and clean the apex, flush it well, do a GBR to build the buccal wall yhicker and taller back to where it should be in the esthetic zone, place the flipper and see them in 4 months to place the implant. There are too many things to go wrong in these cases. Patients are always pushing us to do everything ASAP and in the fewest possible appointments. Many of us have bought into this because we fear patients will go down the street to have same-day-implant procedures. I don't worry about being fast. I take my time. Back out the implant and start over.TomD comments:
Does anyone use the implant osteotomy drills to clean out the sockets of the extracted roots? The medium to large ones...Carlo comments:
what is the material that appears to be sticking to the abutment above the implant collar? Cement? Maybe the problem is not with the implant but with that material deep below the gingival margin causing inflammation.shweta comments:
That is the gutta percha. We had taken x ray with gutta percha placed in sinusprince comments:
looks not sufficient connective tissue buccally,open flap ,remove all infection,put graft and membrane, ,make the crown margins supra gingival,make sure margins are clear of any cement, pt is female?,more chances of gum infection in pregnancyshweta comments:
Thank you all for ur valuable inputs. Since lot of my friends here are in favour of explantation and redo. I do have a question. This seems more of periimplant mucositis to me rather than a periimplantitis seeing the bone levels. So what do you all suggest regarding opening up the flap, debriding granulation tissue, cleaning up implant surface if exposed and then decontamination of the biofilm??? Can this implant be salvaged?John T comments:
(a) There's no reason to suppose 2.2 is non-vital but if you're at all concerned why not vitality test it? 1.1 has lost its translucency and had a chipped incisal edge - presumably traumatised at the same time as 2.1 - and is more likely to have reduced vitality. Doesn't need endo if it's symptomless but worth noting in the records just to cover your back.(b) With this amount of infection around the 2.1 implant it is academic whether this is periimplant mucositis or periimplantis. The implant is a no-hoper and is clearly destined for the bin. Just take it out. Don’t muck about with GBR, etc. Just let it heal and re-assess in, say, 3 months.
You can’t win them all.
otis comments:
off on a tangent here...why not GBR? more chance of infection? complication? or simply or just not needed?doclock comments:
Besides inadequate space to lateral, there is a definite labial problem. You will have to flap and evaluate.