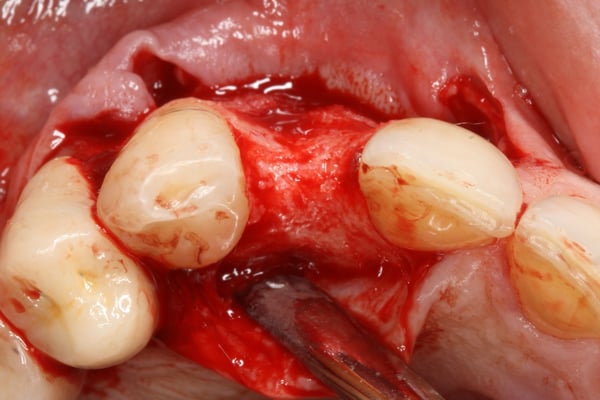
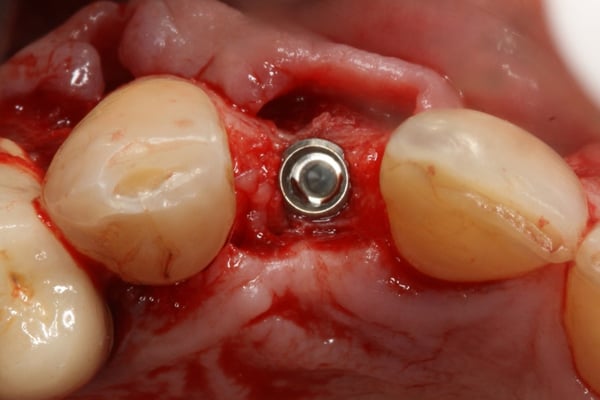
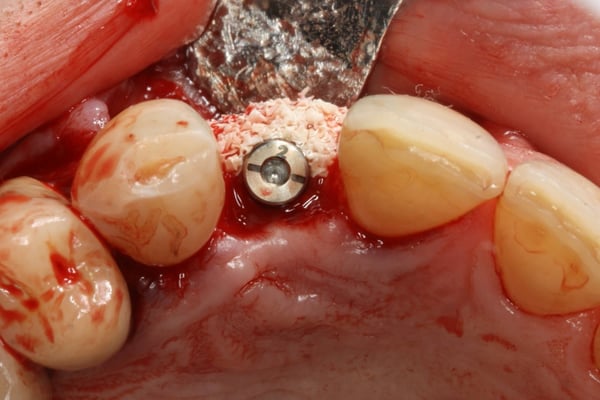
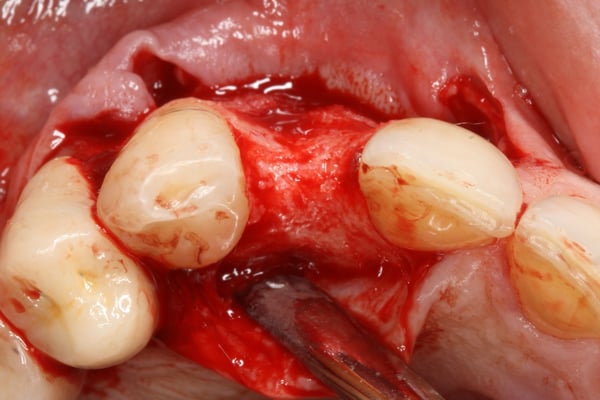
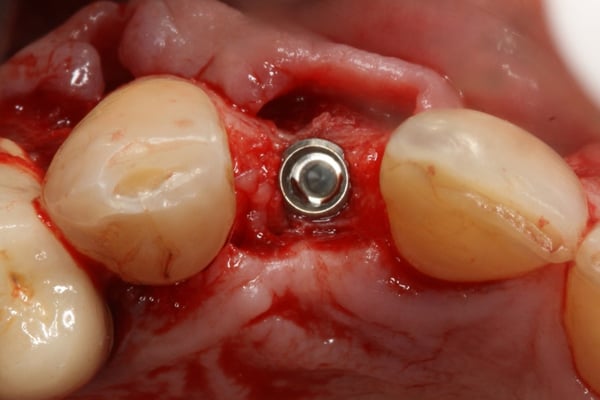
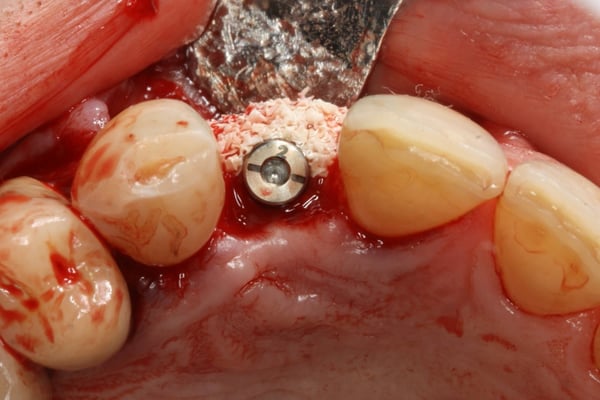
This case video is a continuation of the [Part 1 of Hopeless Maxillary Anterior Tooth](https://community.osseonews.com/t/the-management-of-a-hopeless-maxillary-anterior-tooth-part-i/195) discussed post-extraction socket healing and site development for implant placement. In Part II of the series, we describe the implant placement, provisionalization and final restoration. Despite successful regeneration of the original defect, the contour was obviously deficient and was addressed by employing the "Sandwich Technique". This entailed the use of an autogenous bone layer (see Autogenous Bone Collector or Disposable Bone Scraper ) followed by Xenograft Particulate that is layered over the autogenous bone. Following integration, a provisional was fabricated to shape and contour the peri-implant tissue and a final restoration was fabricated. One interesting topic that is brought up during the restoration phase is the issue of residual xenograft material in peri-implant soft tissue. How to handle the residual graft is still somewhat debatable with some clinicians claiming it should be cleaned out with other suggesting it's good for stability of the soft tissue.


period comments:
Nice Case. Do you expect further papilla regeneration over the next 6 months or 12 months? A follow-up photo at these points in time would be interesting.
drdangober comments:
Thanks so much. I wish I had a long-term follow up photo to share. This case was done over 10 years ago and the patient disappeared soon after the implant was restored. I am not so confident that the papilla would have completely regenerated. I believe as a result of the multiple surgeries and flap reflections there was some interproximal bone loss which would preclude 100% papilla fill unless the contact was raised. What do you think?
period comments:
You're probably right. Many or most patients are still very pleased even when there is a little less than 100% regeneration. I think it is a trait of implant surgeons and restorative dentists to feel pressure for the 100% result. This is part of our nature and it is reinforced by all the AAP and AO presentations we attend showing amazing results in the esthetic zone.
I do generally expect improved papilla form and embrasure fill 6 to 12 months following insertion of the restoration.
drdangober comments:
If possible, would you be able to share a case or two which demonstrate that? Thanks for the discussion!
Good case and great discussions. I have two questions for you:
- Did you take into consideration Tarnow’s predictability criteria for the occurrence of black triangles post operatively (i.e., pre-operative bone level assessment and planned implant position based on this bone level)?
- In the event that this patient did have a high smile line, how would you have gone about addressing the black triangle issue? Would you have considered a soft tissue graft with a long term sling type suture? What are your thoughts on a pin-hole type procedure post-operatively to coronally reposition the interproximal tissue to close the black triangles?
Would love to hear your comments and input on these.
Thanks,
Dr. Ajay Kashi
Both great questions. I think that from a pre-operative perspective, the assessment of the smile line is critical in terms of patient expectations. This particular case had a very scalloped architecture with a “thinner” biotype and the likelihood of maintaining or re-establishing the identical papilla is low. Additionally, bc of the nature of the bone defect and the inability to immediately place and provisionalize without raising a full thickness flap, the likelihood is even less. I do not think a soft tissue graft would help in terms of the papilla since it would not address the interproximal bone levels, even with a sling-type or composite-stabilizing suture.
Had this been an esthetically demanding case with a high smile line, a consideration of additional prosthetics to adjacent teeth would have been indicated to control contours and proximal contacts.
Thanks for your input. Appreciate it.