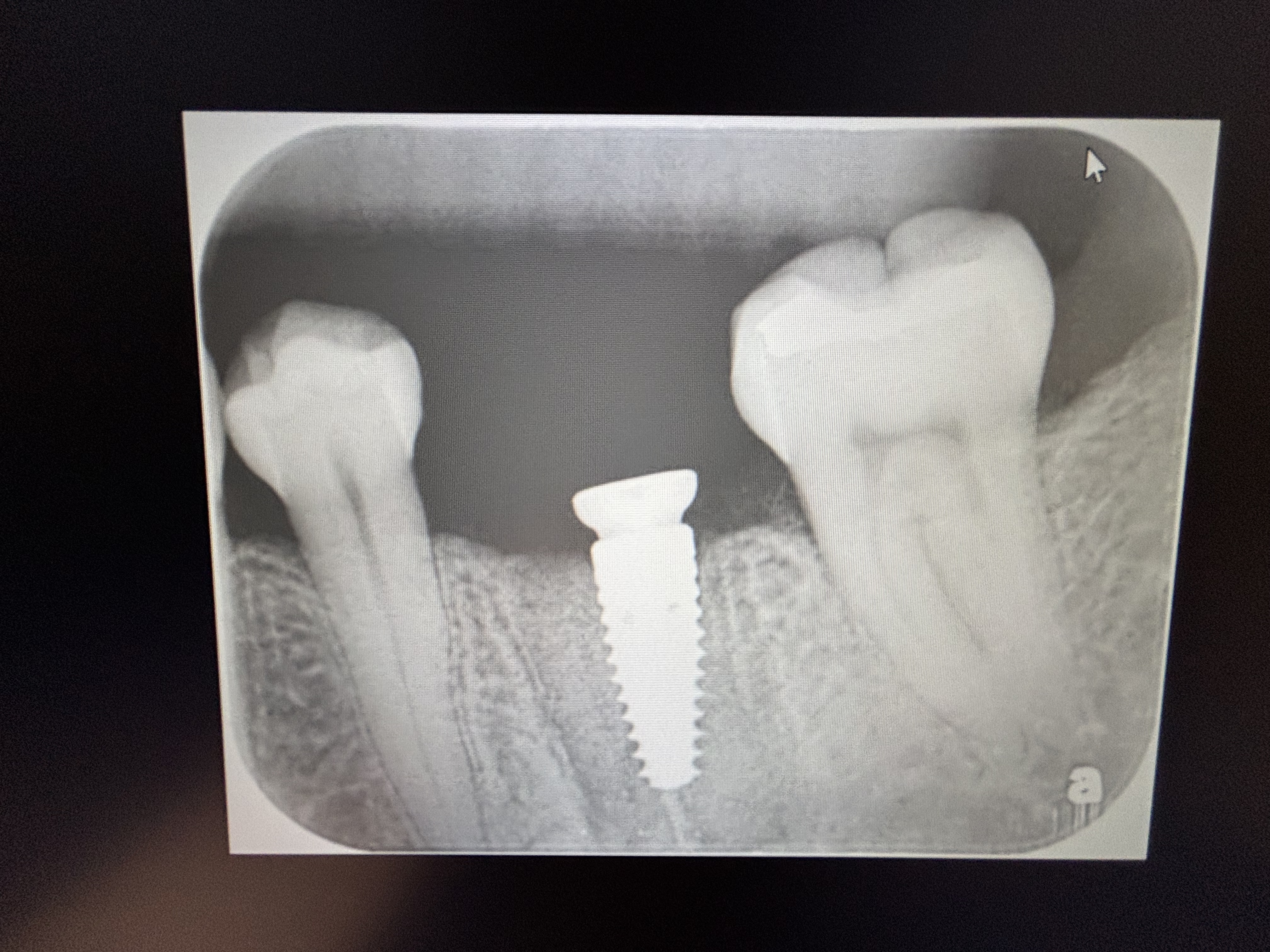
Coronal Bone Loss on #7 Implant: Any Suggestions?
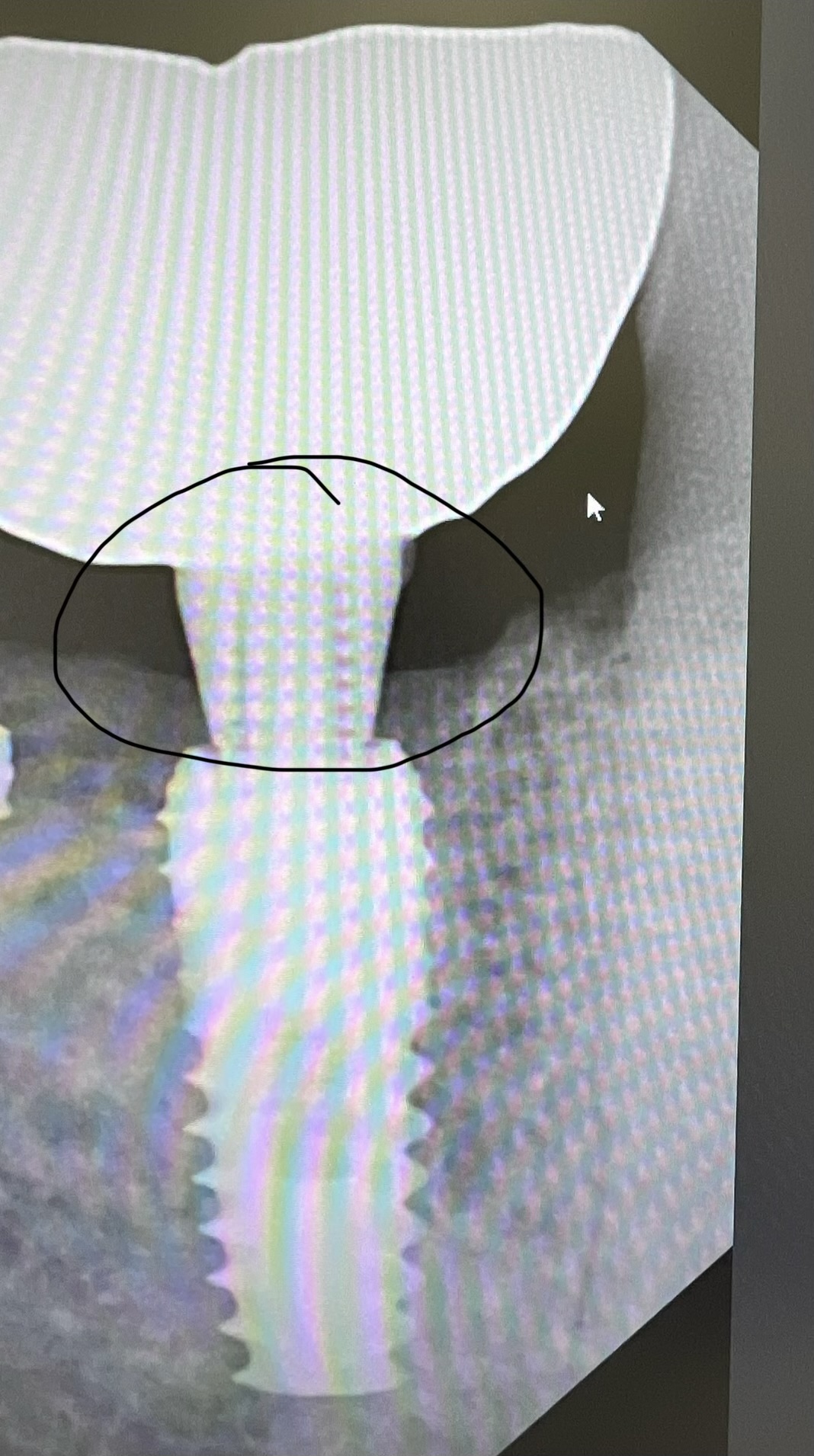
#7 was extracted in April/2013 and an immediate implant was placed (MIS 3.75×11.5) into the socket with a bone graft and collagen membrane. It was allowed to heal unloaded until Nov/2013 when it was uncovered and fitted with an angulated abutment. In Dec/2013, the abutment was torqued and the crown was cemented. In June/2014, the patient returned for follow-up and an x-ray was taken which showed some coronal bone loss. The implant was solid with no mobility. Patient stated that she was taking Fosamax.
Subsequently, a flap was raised, the area debrided, and a reparative bone graft was placed and covered with a collagen membrane and sutured shut. One month later, the patient was seen for a post-op and appeared to be healing fine. One month later, the patient was seen for another post-op and had some exudate present. She was given a syringe and advised to irrigate the area with Peridex, but was not improving over the next month. In Sept/2014, since the implant was still about 60% anchored in bone and not mobile at all, it was decided to just trim the gingiva mildly and smooth off the threads that were exposed above the level of bone.
The patient was seen for follow up in Sept/2014 and again in Dec/2014 and again in March/2015. In all instances, the implant and the surrounding tissues appeared fine and asymptomatic. However, in June/2015, the patient returned complaining of exudate. She was placed on Doxycycline for 10 days and we reviewed oral hygiene, and stressed the need to irrigate the gingival pocket daily with Hydrogen Peroxide 3%. The patient was seen again in July. The implant is still solid with no mobility and has maintained 5 – 6 mm pockets. The gingiva appears pink and firm but still has some exudate present.
Any suggestions for this case?