Early peri-implant bone loss: normal response?
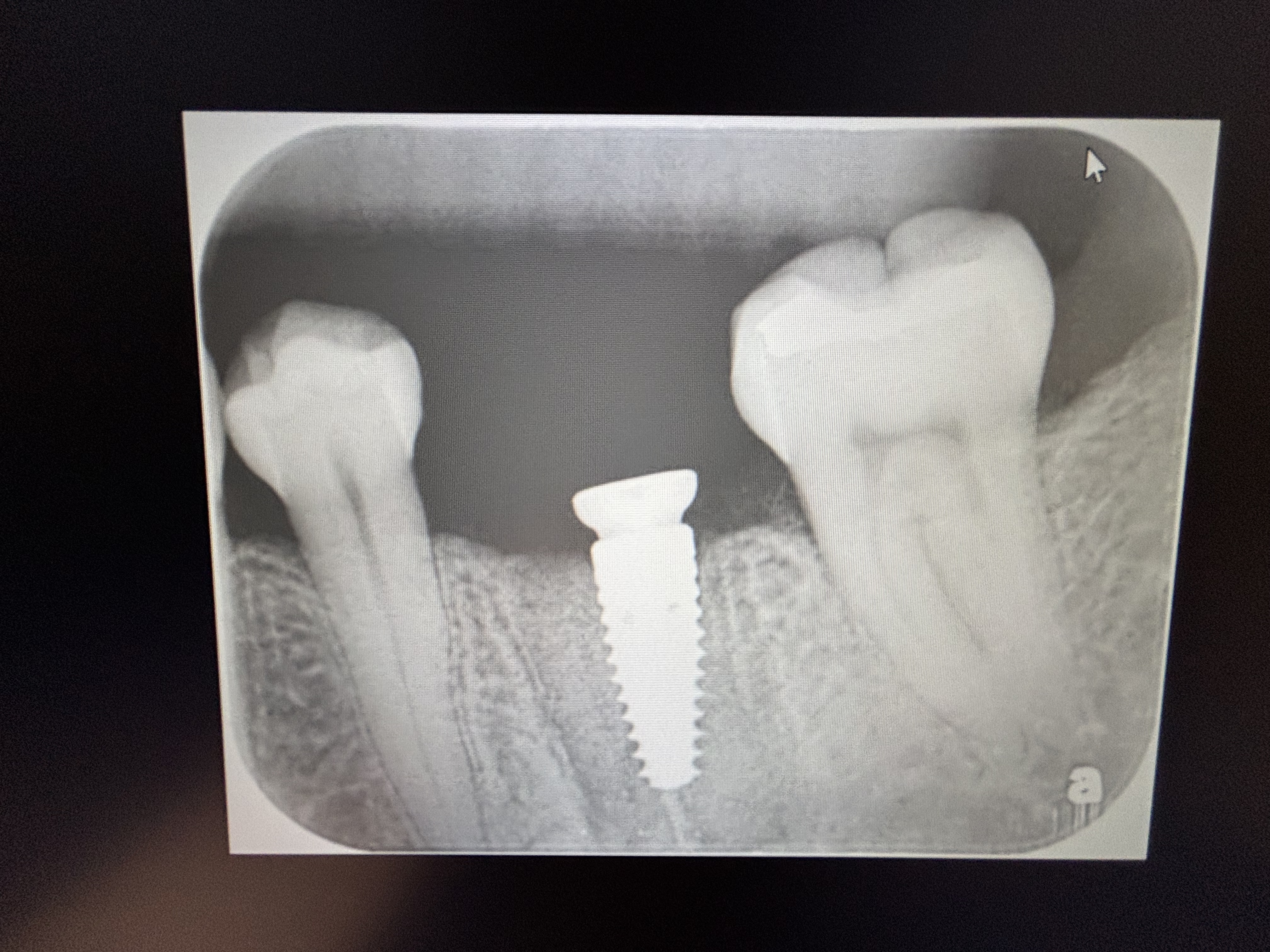
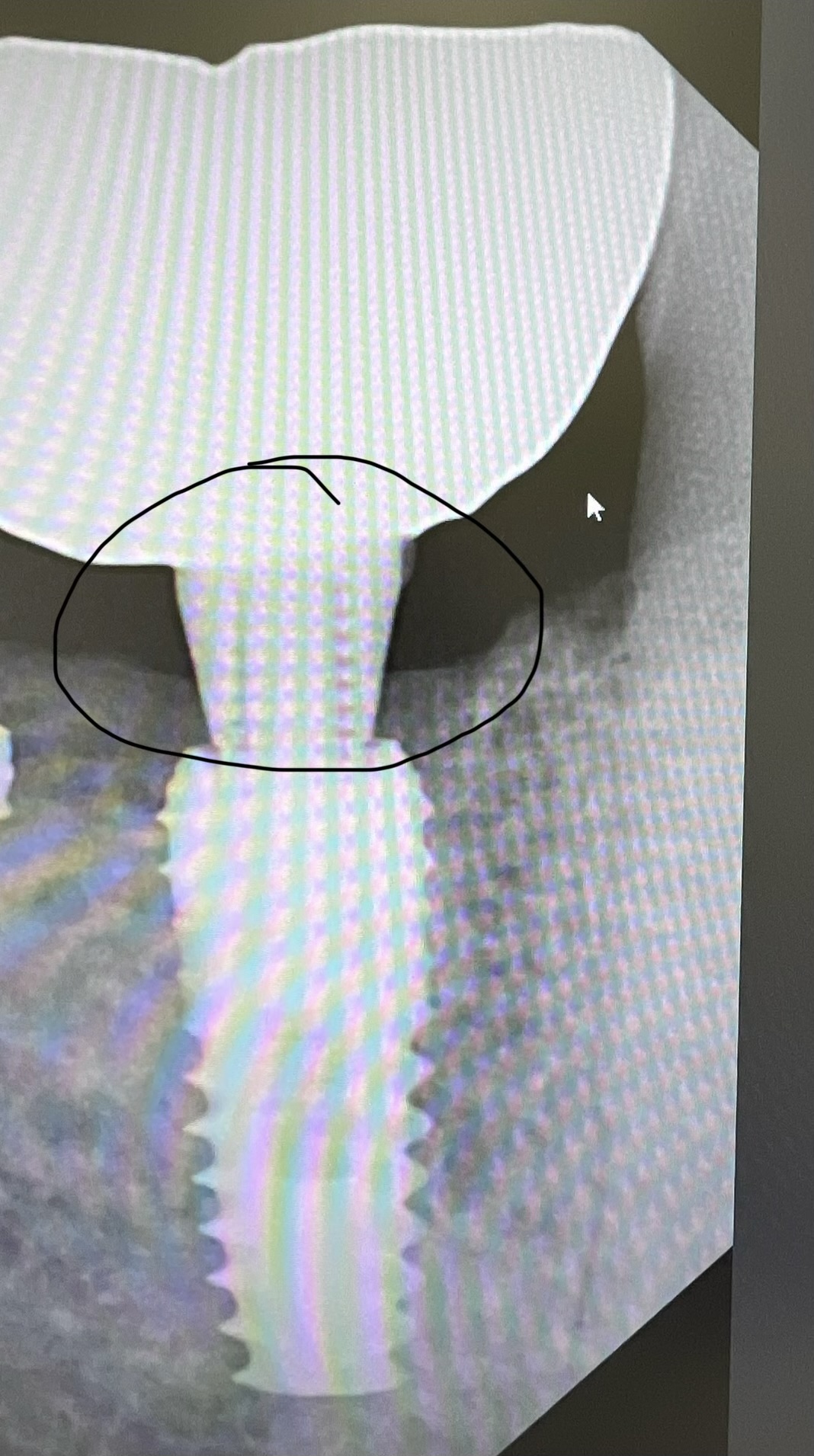
I have a 67 year old female patient who smokes 10-15 cigarettes a day. She has excellent periodontal health. I installed implants in an edentulous area in #19, 18 areas [mandibular left first and second molars; 36, 37]. On the 1 month recall the healing abutments were exposed. I changed the healing abutments. The radiograph showed rapid bone loss around #18. Is this a normal response of the bone? Could this bone loss be due to cigarette smoking or overheating the bone when I drilled the osteotomy site?
![]peri](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2014/04/peri-e1397071061154.jpg)
![]pano](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2014/04/pano-e1397071083729.jpg)
13 Comments on Early peri-implant bone loss: normal response?
New comments are currently closed for this post.
CRS
4/9/2014
Watch carefully they don't seem to be intra grating. Four to six weeks is key
Anton Andrews
4/11/2014
I would remove the distal implant and placed a wider one 7X7/8 combined with the graft using Russian AAA technique. The mesial could be grafted. One surgery for all.
CRS
4/12/2014
Is the patient wearing a flipper or partial over the surgical site, that could be the culprit. In this patient I would have buried the implants and placed flat healing screws to keep the implants protected during osteointegration the patient could even be chewing on the exposed healing heads. Any grafting if intervention at this time will fail if the preceding factors are true. When you see bone loss this early the implants are not integrating, surgical technique, overheating, high torque and smoking are all possibilities. Is the patient on any meds Bisphos, or have any issues with calcium metabolism? The list can be large. One thing I can say for sure your implants are not integrating, they are failing. If it were me I would remove come up with a reasonable diagnosis if why they failed and start over. The factors I listed should help. Triple A Russian or any other technique will not help until you figure out what happened first. Sometimes the biology need to be looked at first vs being a technician that's why we are doctors.
Ed
4/12/2014
No removable prostheses, but the distal one has an accidental exposure at the first two weeks. I think was an easy surgery, with no high torque insertion or bone overheating. The thing is I have seen results like this in some cases in literature; thats the reason why im so worried about this response to the bone. Perhaps accidental exposure is something more than negative for the correct healing of the surgery, combined with no smoking cesation patients. Is my first impression for this failure.
CRS
4/12/2014
If the exposure is small like thin mucosa over a healing head then we just maintain it. If the flap breaks down it could be infection, poor bone quality, or the smoking. I'm also a little nervous over the anterior implant also. The back implant may need to be removed, grafted and try again or use the middle site. Smoking may also be the culprit since it is so hard on healing tissue.Also rule out any medical causes. I would try again but warn the patient that she may not be a candidate especially with the smoking. Do you know how the teeth were lost?
Ed
4/13/2014
She was wearing a bridge from 34 to 38 With a fracture of the endodontic mesial abutment and of course I extracted the distal abutment too with a big traumatic defect on the mesial side.The rx image show a radiolucency in the mesial implant but is really the defect I could see in the surgery, that can be seen in the orto of the day of surgery. Im following the healing and i think this implant is healing well. Also, this implant is healing in two stage procedure with no exposure of the cap. Thanks for reply the case "CRS", im very worried about complications in my clinical practice that i cant find the reason, such cases like this. Do you think is really an option to graft in a site where a progressive bone lost can be diagnosed?
CRS
4/13/2014
I think and this is anecdotal but I am finding this complication consistently with failing endodontic teeth. Could you post a preop photo. If this is the case what I am telling my referring docs is to have me remove the teeth since I use my Nd-Yag laser 1064 wavelength to kill the pigment containing bacteria which are sequestered in the bone. It has to be this particular wavelength diode, tetracycline erbium,etc won't penetrate. When the implant osteotomies are cut these bacteria are re-exposed. My protocol is to remove failing teeth or implants and treat with the laser. So far so good, I may be on to something here. The common thread appears to be the failing endo and the pigmented bacteria also the timing on the failures. It can't hurt to graft but if the bacteria are still there the process will continue. The laser seems to do the trick due to the wavelength and depth of penetration which is unique.
DrT
4/15/2014
It does not appear that you placed the distal implant at the level of the osseous crest. Do you have an image taken at the completion of the surgery?
David Vaysleyb
4/17/2014
I often have problems w/heavy smokers.
@CRS- Very interesting about the Nd-Yag laser. I will have to read up on it more.
I have had good success w/flapping affected area, gentle curettage, apply sterile gauze w/hydrogen peroxide 3% (standard from stores) for 2 mins, then graft w/a mix of tetracycline (can't buy it anymore here in the USA) or doxycycline and allograft cortical-cancellous (.25 to 1) bone. Cover w/membrane and pray!
So far this has worked fairly decently. I have maybe 2-3 cases a year like this.
David Vaysleyb
4/17/2014
@CRS- what was your old protocol for failing endo teeth? Curretage w/surgical spoon?
Some baseline would be appreciated. Before and Now.
Recently, I've followed the curettage and irrigation protocol. Then take up a surgical handpiece w/medium rounded shoulder diamond (size 1.4mm) and reach into the deep nook and crannies of the EXT site. I also de-epitheliaze 1-2 around the sulcus of EXT site. Very low speeds.
So far (last 6 months), this has worked well for me.
CRS
4/17/2014
Actually I have quite a bit of experience with this. Until root canals were done with a microscope many canals were left untreated so my apicoectomies were doomed to fail in a year or two. Fractures were missed also. Now with 1064 laser I can disinfect the pigmented bacteria which are just under the osseous surface which the hydrogen peroxide won't be able to get to. So you see it is a progression of surgical techniques and understanding the biology of the area not just a mechanical cleaning with a spoon. I don't use antibiotics in grafts it is toxic to new bone growth. So actually my protocol for apicoectomies is retreatment with a doctor who is experienced with a microscope. If there is significant pathology then an apicoectomy. The microscope eliminates untreated canals and patients with unresolved post root canal pain. The laser gets rid of residual bacteria when I remove the failing endo. The problem is when the implant is placed the bacteria are re exposed. So a perimplantitis may develop. Root canals are a great treatment modality when performed under a microscope, you can't treat what you can't see. That's my bias.
Gregori Kurtzman, DDS, MA
4/22/2014
Do you have a radiograph taken immediately following placement? (a PA)
DrD
4/22/2014
I think the topic is covered sufficiently. I wanted to add one thing however. In the over 25 years of practice(half of those placing implants) I will see a large implant failure rate in smokers. IF I cannot get the patient to cease smoking I tell them they are looking at a 50% failure rate. I've had numerous locator or over denture/ hybrid cases where one will integrate and one will not. Same surgery date, same protocol, same arch. Nothing to chalk it up to except that the patient is a smoker. I have virtually no failures otherwise. Smoking is the death knell to integration. I prepare them for this fact and tell them I'll gladly place another one after the site heals however they will pay me again for the failure as it's not my fault but theirs. A lot of surgeons I know refuse to place in smokers, period. I really wouldn't rack your brain about it. Non integration occurs routinely in smokers, bottom line.