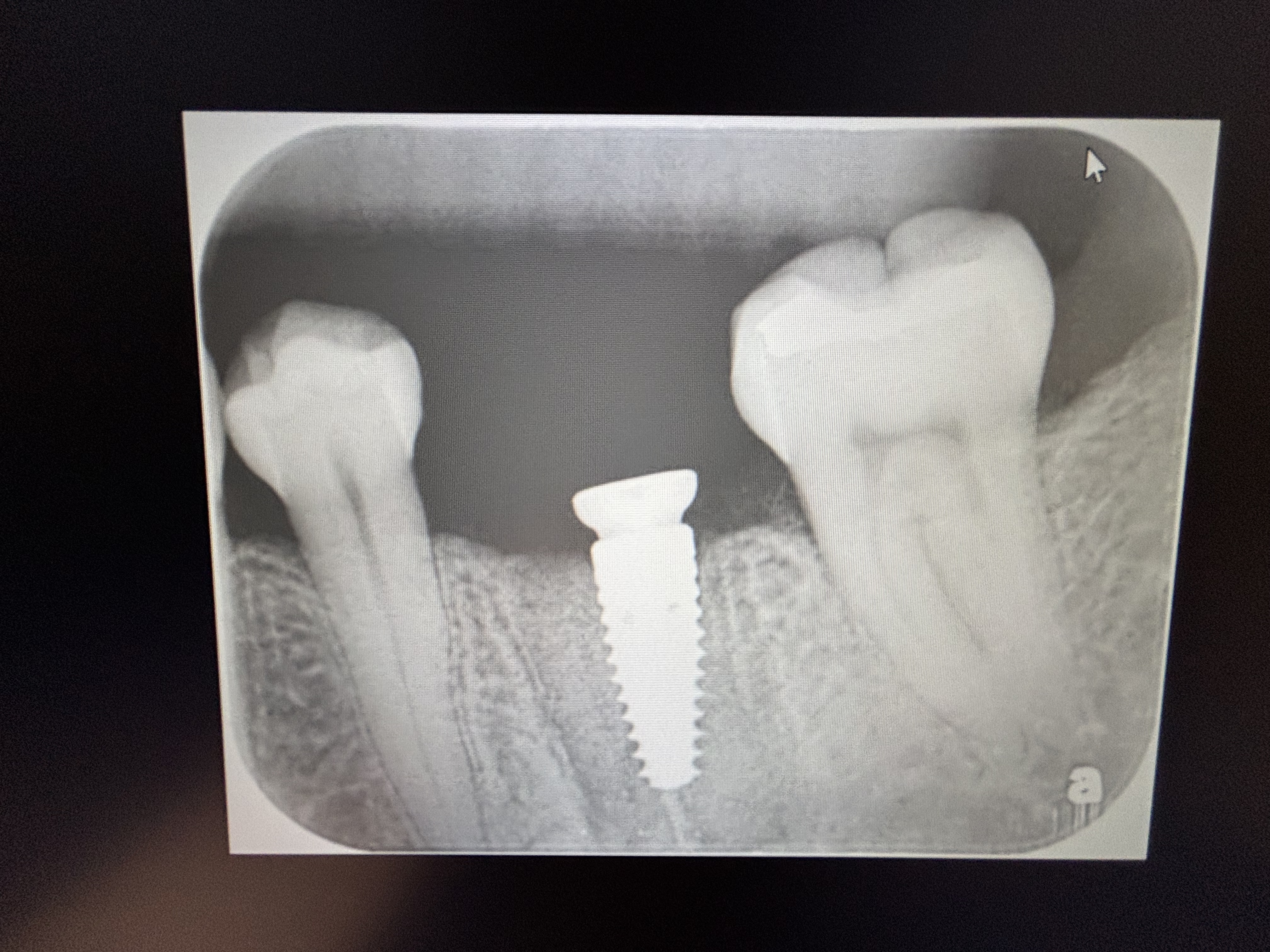
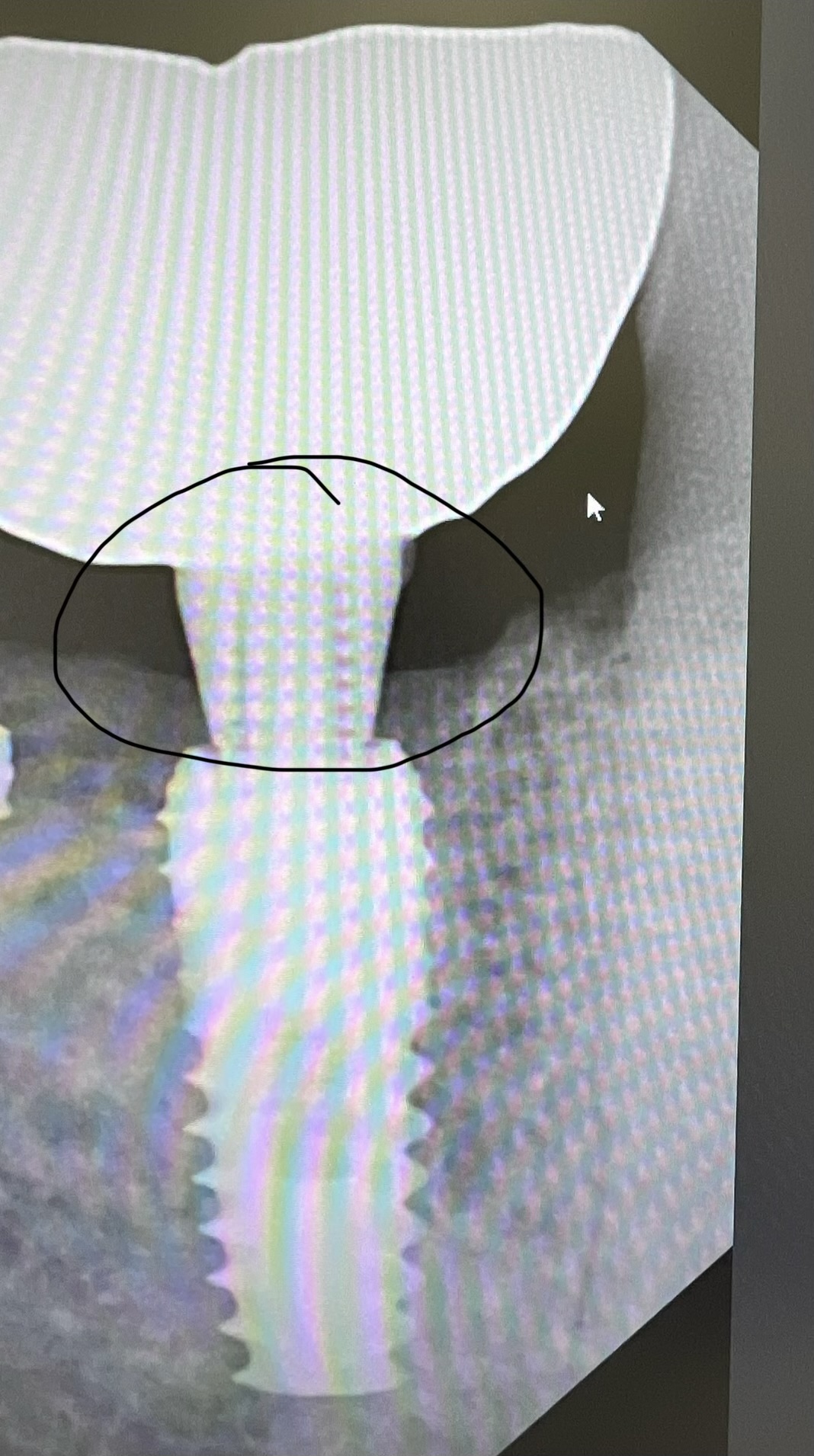
Graft Material Appears Gone: Suggestions?
Dr. B. asks:
I recently placed a 4.3mm diameter Nobel Biocare tapered groovy dental implant immediately upon atraumatic extraction of #10. Using the “Bio-Col” technique with Bio-Oss to graft the gap between the socket walls and implant, I was able to engage about 5 mm of fresh bone beyond the apex of the tooth. Therefore I got excellent initial stability greater than 35Ncm. However, upon return 1 week later, there is exposure of the cover screw and the Collaplug and graft material appears to be gone? Any thoughts? I welcome your comments/suggestions.
12 Comments on Graft Material Appears Gone: Suggestions?
New comments are currently closed for this post.
satish joshi
12/17/2007
Forget about all other factors.
Just think aesthetically.Think of the difference between FINAL RESULT of leaving same implant and removing it,and rebuilding the site and then placing new implant.
Dan Holtzclaw, DDS, MS
12/17/2007
What was the original HDD (Horizontal Defect Distance) between the implant surface and the buccal plate?
Dr. B
12/17/2007
not uncommon in cases of immmediate implant placement
primary closure or delayed placement is safer
Dr. Ben Eby
12/18/2007
First, forget Bio-Oss in these cases. It takes too long to resorb and turn into bone. Use DFDB, or nothing. The Colla Plug is a little dense to make an effective clot. If the interdental pappilla is intact and the labial plate is intact, you can place the implant within to socket with primary stability. Place it at least 2 mm lingual to the gingiva and 3 mm below your expected labial-gingival margin, and place a straight 3 mm healing cap on it. (If you wish, and I often do, place Grafton in the socket prior to placing the implant, letting the excess sqeeze out). Instruct the patient, not to use any chemicals in the mouth, including tooth paste till the one week post op check. Make sure your temprization do not impinge on the healing cap, even under load. The patient needs to be very careful about any kind of implant micromovement for at least 6 weeks, the time it takes to get back to your initial stabalization.
In this case, if you have exposed threads and the ultimate result does not look promising, you may be better off removing the implant and grafting the area. Then wait for 4 - 5 months and place the implant and additional graft material as needed. If in doubt, get some help.
Dr. Ben Eby
12/18/2007
Additionally, I sometimes use a wide bodied 3 mm healing cap if I need it to support the interdental pappilla and feel the the gingival height in relationship to the other anterior teeth is ok, and will be ok if I loose about 1/2 a mm.
jabern
12/18/2007
dan: the inital distance between implant and the buccal plate was about 3mm
In response to Satish: thanks for comment. However, if implant remains stable I will tend not to remove. I intend to just place a healing cap now.
Dr. JB
12/18/2007
Sounds like another immediate placement hiccup....there is a time and a place for immediate placement....also sounds like you had a lot of osteoclastic activity and no osteoblastic activity....throw away the Bio-Oss....go with a Demineralized Bone material with low CA content....this will up the BMP's!
Also stop doing immediate placements! I learned my lesson and I wish everyone would about that sort of procedure....it is too unpredictable!
Rand
12/18/2007
Dr. Eby gave excellent comments. I would only add the following:
The integrety of the blood clot is paramount. In these cases I have given up using local anesthetic with vasoconstrictor. I want as much bleeding in the area as possible. Instead of collaplug, which will disintegrate in a week or two, I use a collagen membrane that will last longer. I suture the collagen membrane in place and cover it with coating of suture glue. I do not want anything distubing the clot. If the clost stays, the graft will stay, almost always.
If there was any hint of infection, I would probably have grafted first and placed the implant later.
Dan Holtzclaw, DDS, MS
12/18/2007
I do immediates all of the time in the anterior. The problem most people run into with implants is lack of planning. They see a hole and they want to fill it.
I don't think the problem had anything to do with osteoclastic or osteoblastic activity. It sounds like your graft simply dislodged. Look at the wound healing literature. You will see that the clastic/blastic argument does not hold water.
Not all situations are correct for immediates. You need to establish a set criteria for when and why you want to do an immediate implant. There are a multitude of factors to consider.
All too often, people see a hole and they want to fill it with an implant. There is little planning and the end result is a disaster.
I had a patient come in the other day with an implant at site 31 (US). Let me tell you about this implant. First of all, the crown was loose. Why was the crown loose? The crown was loose because the abutment screw fractured. Why did the abutment screw fracture? The screw fractured because it was way too long for the implant. Why was the screw too long? The screw was long because the abutment was huge. Why was the abutment huge? The abutment was huge because the platform of the implant was placed much too apically. This implant had a crown that was about the size of a premolar. It was placed in crossbite. It had terrible occlusal interferences creating off axial loading. This, combined with the excessive length of the screw, is what most likely led to screw fracture. On top of this, the implant had peri-implantitis due to a 7mm probing depth. The 7mm PD was related to the platform placement and soft tissue profile.
So, this patient paid a few grand for an implant at a site that is occluding with maybe 1/4 of a tooth. Is chewing efficiency improved? NO. Are esthetics improved? NO. What was the point of this implant?
This implant was doomed from the start because the dentist that placed it failed to plan. They simply saw a hole and wanted to fill it. Now, I have to clean up his mess.
Back to the original question, if the HDD was 3mm, you were correct to graft. I would not have used BIO-OSS. Just my personal preference. I find that it sticks around much too long. I prefer to use a human allograft. How did you temporize the site? I have found excellent success with using a resin bonded bridge type temporary. If I am doing an immediate, I will retain the patient's clinical crown, add composite to the apical portion of the crown to create an ovate pontic, and then bond it to the adjacent teeth. This temporary pontic provides the ultimate in esthetics, supports the papillae, and protects the graft site.
Dr. B
12/19/2007
i don't think it is related to osteoclstic activity too. bio-oss is almost non resorbable and will stay there for life. it just come out of the wound when the collaplug resorbed.
Dr T
12/19/2007
I always build up my bone first. But there is also a possibility to lose the bio-oss. You have to drill some holes in the spongiosa to get a good receptor field for the bio-oss. Just putting some bio-oss against the buccal boneplate will not intergrate and with no good closure you lose the bio-oss. In your case I will take out the implant and build up the bone first. Good luck
PK
12/19/2007
Do not bother grafting Bio-oss or what ever, unless you know how to do primary closure.Follow Dr.Joshi's advice.It will be better for you and patient.