Implant Fixture Too Close to Root of Adjacent Tooth: Will it Osseointegrate?
Anon. asks:
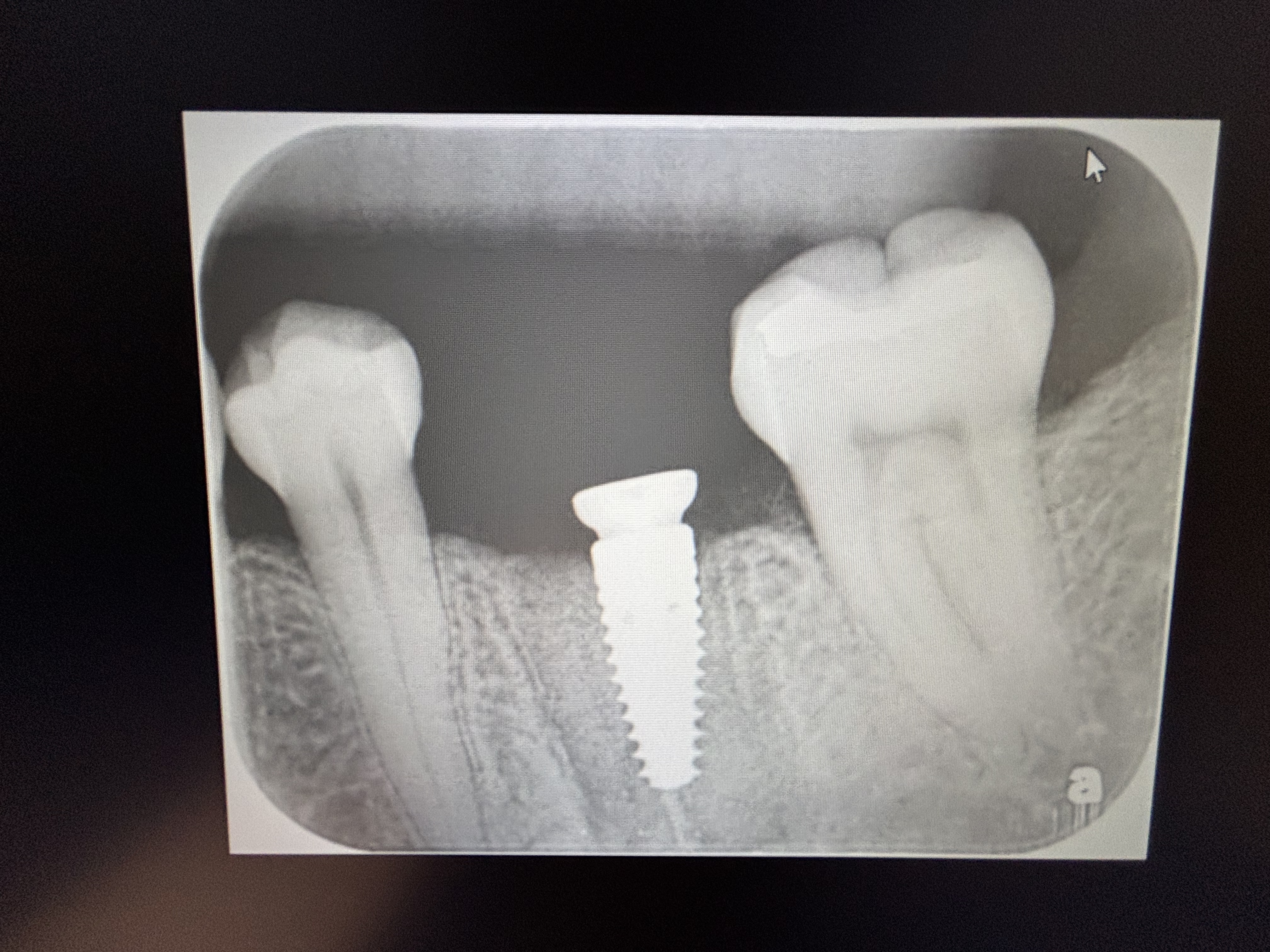
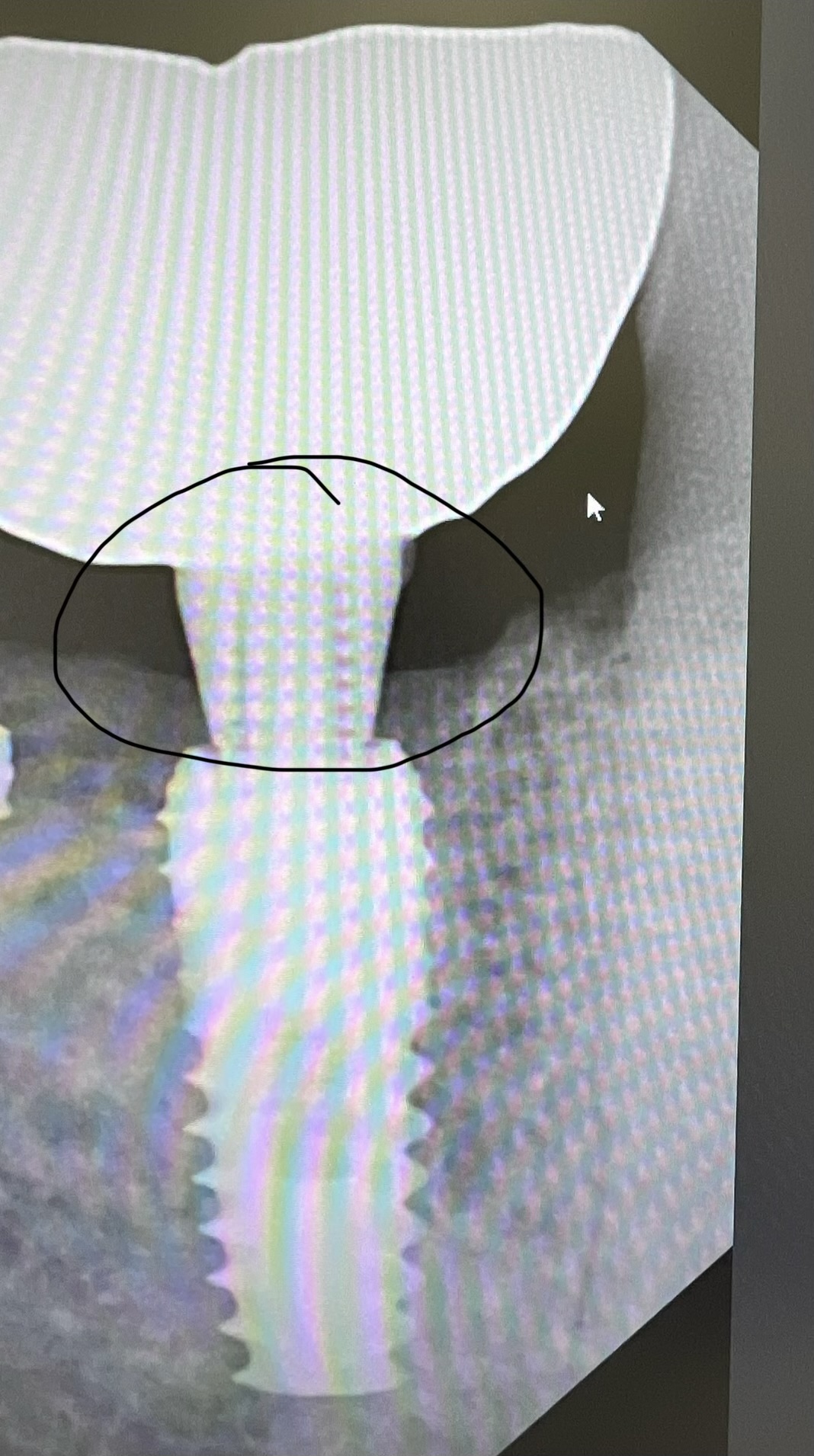
I placed one implant on the #13 site [maxillary left second premolar] but underestimated how far from the maxillary first premolar I should have drilled the pilot hole. When I realized that I was 1mm away from the root of the maxillary first premolar [#12], I tried to reorient the pilot drill and drill again. But even after this attempt at correction, the implant fixture is too close to the root of the adjacent natural tooth. If I leave the implant fixture as is, will it osseointegrate? Or should I remove it, bone graft and try again, this time, not so close to the adjacent tooth. I think the root of the first premolar curves and I did not realize this in studying the per-operative radiographs. Any thoughts>
30 Comments on Implant Fixture Too Close to Root of Adjacent Tooth: Will it Osseointegrate?
New comments are currently closed for this post.
UW Perio
8/25/2008
The implant will most likely integrate. The questions you should ask are: Is it restorable and will the premolar require endo down the road?
charles Schlesinger, DDS
8/25/2008
In a ddition to what was pointed out above, if you are left with less than 1.5mm of bone between the implant platform and the adjacent tooth you can expect a loss of bone between your implant and natural tooth which will result in the loss of the papilla. Did you take a check film after you drilled your pilot hole? That should have given you some indication that you were may have been too close.
Neda-Moslemi
8/26/2008
I agree with UW Perio.
If the distance between implant fixture and adjacent tooth is sufficient in coronal part, do not worry about implant clinical sucess, but endodontic treatment will be probably required. Please follow your patient and test the vitality of the first premolar tooth once a week and do RCT whenever you find it non-vital.
If the entire length of the fixture is too close to the root, implant removal is recommended because it will not be restorable even if it is clinically fixed.
Is the postoperative radiograph available?
RIk
8/26/2008
I agree with all the above comments and also wanted to add that even in simple cases like this, a Cone Beam CT might have given you a better mental picture as to where the adjacent root was going and might have influenced your initial trajectory...
Rik
Bruce G Knecht
8/26/2008
It is hard for us to comment without seeing a PA. Another thing that needs to be seen is the depth of implant placement to the CEJ of the adjacent tooth. A good idea is to take an impression of the implant before it intergrates, and have a lab PEEK aboutment and temp made and see if a papilla can form. The stone model will give you the best perspective if this will work or not and you will know with the tissue healin in a month if it will be a doable thing. Good luck.
Dr.Rajesh Bhatia
8/26/2008
We had a similar case where we placed a implant at the site of #14 very close to the roots of #15.It healed remarkably well.So leave it .Just explain the pt. that he might hv to get the next tooth endo. treated
Chan Joon Yee
8/27/2008
I think a perio problem would be far more likely than an endo problem.
Juan F. Aragon
8/27/2008
What its the reason to do an endodontic treatment in cases like this?
Thanks
dr ACatic
8/27/2008
Unfortunately I had the same problem about a year ago involving implant in position 35 (lower left second premolar) placed in the apical part cca 0.8-1mm to the apex of the tooth 34 (lower left first premolar). I must have injured blood supply to the 34 and about 2 weeks postop I had to do the endo on 34. At the CEJ the tooth-impl space was 1.8mm and no problems later. Didn't do the post-pilot drill x-ray due to faulty equipment at the time. Needless to add, don't do a thing without it afterwords.
Dan Holtzclaw, DDS, MS
8/27/2008
You need to consider a few things.
1. Platform location. If the platform is too close to the adjacent tooth, you will have restorative problems and you will lose the papilla. Another factor to consider is the platform relationship to the adjacent CEJ's. If it is too coronal, you will have restorative problems. If it is too apical, you may end up with periodontal problems down the road.
2. Apical location. If the apical portion of the implant is too close to the root, you will probably be ok so long as the implant is not grossly penetrating the adjacent root. I would monitor the adjacent tooth for any signs of pulpal pathosis. If any develop, an RCT may be indicated.
3. Sure, a cone beam CT may give you a better idea of the site anatomy, but I feel that is overkill for a single implant site unless you had concerns about osseous anatomy (ie. ridge width or undercut), pneumatized maxillary sinus, or if you were worried about IAN proximity. It sounds like your problem began with the pilot hole placement. Did you have a surgical stent? This would have likely eliminated your pilot hole location error. If you are new to implants, a surgical stent is highly recommended. It takes many many implant placements to develop an "eye" for placement without a surgical stent as you must consider multiple angles (buccal/lingual, mesial/distal, apical/coronal) in addition to monitoring vital structures. Even with the most experienced surgeons, placement without a stent sometimes results in less than ideal implant placement.
satish joshi
8/27/2008
Best solution is to remove implant before it integrates,graft the site and and wait for 4 months to place another one,if you really want to provide better service to your patient.Any thing else would be a compromise restoratively,esthetically,and functionally.Future perio and/or endo(adjacent tooth) problems are real possibility which may lead to implant failure.Apart from not using a surgical stent,this kind of problem may arise some times due to dull drills following old socket walls with two maxillary bicuspids's roots in close proximity and not letting you drill in proper direction.
Good luck.
Dr.Serge
8/27/2008
i got something similar sometime ago...i placed a second molar implant and the body of the implant was touched the distal root of the first molar, the implant was coronally 3mm away from the implant but the distal root was going distally with a big convexity, soo part of the implant touched part of the tooth but fortunately with no problems...
i hope yours also won't have any problem...
Dr.Behnam
8/27/2008
hi,
if the adjucent root is not touched by fixture of new implant and if the
signs of vitality od the natural tooth is positive,i think nothing should be done,esthetic problems can be resolved at the time of prosthetic phase,and remember that integration will be enough at least in 3 parts of four walls of your implant .so if the initial stabilisation is good and after 4-6 weeks post operative signs are normal let the paitent free from the stress of a new surgery,good luck
R. Hughes
8/27/2008
The best way to treat this is to replace the implant in the proper position. Thus,catch it asap and avoid the later issues. I am sure this has happened to alot of us. It has to me, and it's a hard lesson. Even with a good guide it can happen. It does yield aesthetic issues. So try to catch this problem at placement surgery and correct. You most likely will have to us a graft material resorbable and or nonresorbable! Like I stated earlier, this has happened to alot of us, so don't beat yourself to death, learn from it. Have your assistants help you with angulation and use the guide pins, abutments etc. depending on the system one is using.
Peter Fairbairn
8/28/2008
After 17 years of placing I still always take a pilot bur radiograph at 3mm to check angulation and am amazed how many times a correction is required. You can never know all the time like flying in a cloud.
Clark T. Barco
8/28/2008
I saw a case similar to this several years ago where the adjacent tooth was touched by the drill. It took 3 years -- after endodontic and periodontic treatments – for the tooth that was "violated" to be eventually lost. As mentioned, the roots curve, and fixtures are straight -- aligning the stint only with the clinical crowns can, with certian cases, be very deceiving. (See review in J Periodontol Vol 79, No. 8, Aug 2008, page 1324 -- for a similar case.)
That's why we too take an intra-operative radiograph to check our direction (similar to Dr. Fairbairn, but at 5 mm for us) -- it's kept us out of a lot of troubles!
Also, the more we do 3-D imaging, the better we like it.
Dr.Rajesh Bhatia
8/28/2008
Actually even if the osseointegration occurs the real problem is crown placement.Thanks
eric wallace
8/30/2008
Dr. Joshi has spoken the ultimate wisdom. Take the fixture out, graft, and do it better next time. It is so much easier to fix the problem now than get involved in endo, perio defects, long, painfull discussions. Your fixture will integrate, but then you are stuck with it. It took me a long time and thousands of successful implants and many not-so-succesful ones to realize this, but it is really the best thing you can do. Take it out, ASAP. Be honest with the patient, and plan better next time.
Dr. J
9/2/2008
Remove the implant right away. The implant will likely be fime but once you place the crown on the implant the bone loss will advance done the root of the natural tooth to where the tooth to implant distance is more than 2 mm. This problem will not happen for a year or so but it will happen. Papilla loss etc as also another problem.
dr.e
9/2/2008
I agree with taking radiographs to check the direction of your pilot drill. Even when you have a lab made surgical stent ,which is made only considering the shape of the crown and not the shape of the root, you can still get very close or hit the adjacent root. Once this happens you are violating the PDL space and you will have perio and/or endo problems.
This could be used against you in the court, since it could have been an avoidable situation.
So I recommend, taking check radiographs even if you have a surgical guide.
Dr Delendas
9/3/2008
This incidence gives us a nice opportunity to comment on the importance of periapical X-rays before insertion of an implant, especially when this is done adjacent to a tooth.
The main reason is that panoramic x-rays sometimes do not reveal clearly the apical portion of a tooth, which may curve distally or mesially or may present with a periapical pathosis,that could harm the implant in the future.This is especially true for canines.
So do not underestimate the power of a simple periapical X-ray.
sherif hayati
9/7/2008
it happened to my twice may be a year ago,surprisingly i got away with it the first time when a maxillary second premolar was injured while drilling a first premolar implant it went ok even the prosthetics. the second time it wasnt that smooth as epical root resorption occured and i mhad to sacrifice the tooth ,so again ,intraoperative xrays and preoperative 3D is realy usefull.
dr.Alex
12/16/2008
i had the some problem one and a half year ago when i put an implant in position 1.4(upper right premolar).it was at 1 mm from the canine.everything was more than ok.i didn't have any problems with the prosthetic part or with the canine(endo, perio, etc)or with papilla.again at the begining at this year due to the bone quality, old tooth position(i made the extraction)and the mandibular hole i was obliged to put an implant very closed to the apex of the lower right canine.on the x-ray the implant was very closed to 1/3 apical part of the canine.yet nothing happens with the canine.so i was lucky or is not really a problem to be very closed to the radix of a tooth ?
the major problem is when you hit the radix.in that situation for sure you must remove the implant and try another direction.
Dorian Hatchuel
12/31/2008
A comment regarding your reorintation, unsuccessfully, of your pilot drill.
Sometimes it is not possible to use the pilot drill to reorientate especially if your space is limited. Buy yourself a Linderman bur which is a side cutting bur. Cut the bone sideways and then reinsert the pilot drill. I have one of these burs in every implant tray as a standard. Very useful.
Dr. Veta
2/18/2009
I placed an ITI SLA surface implant two months ago in position of tooth #19 (36 for ther FDI system.IT was a 12mm long and 4.8 wide implant.I did not do the block, just in case I was in the proximity of the inferior alveolar nerve, although I could measure at least 15mm between the alveolar crest and the inferior alveolar canal. The patient felt pain while drilling.Although I took an X-ray with a direction indicator at 11mm which showed that I was 3mm away from the nerve, I only drilled at a length of 11mm for the 12mm implant, because the patient was complaining. As a result the implant is placed approximately 1mm more coronal than it should have been.Now that the patient is having the implant restored complains about the metal showing on the buccal aspect of the implant shoulder and the wide embrasures on the mesial and distal of the implant.I talked to the people in the dental lab and they say that they can extend the porcelan more apically to cover the implant shoulder.Should I have them do that, or it will cause problems for self-plaque control?
The patiend is a 33 year old healthy male with healthy periodontal tissues.The probing depth around the implant is 2-3mm. No titanium surface is exposed, but when I probe my probe reached the titanium surface.
R. Hughes
2/19/2009
Dr. Veta, You can prep on the implant, impress and later cement a nice esthetic pfm crown. No bid deal.
Dr Marvin Cota
4/18/2009
take rvg in different directions one from mesial and one from distal to confirm proximity to adjacent roots
you may be surprised to find you were actually a good mm away
vancouver
4/18/2009
do other people agree with prepping the actual implant to cover recession? I can see how it may work, however possible future retrieval may be problematice. I am not sure how comfortable I'd be drilling the actual implant.
Recent Implant Patient
9/16/2009
I'm a little disturbed by the degree of clinical distance in this discussion in regard to the patient's requirement for future RCT or "sacrifice" of the adjacent tooth and the subsequent pain and disruption to his/her life because of an error in judgement during implant placement.
I had an implant to #13 2 weeks ago and while so far the gum is healing well over the implant, I'm experiencing extreme pain in #12. During my implant surgery, my surgeon re-placed the implant three times before he was satisfied with the placement. I'm hoping that the pain I'm experiencing is transitory due to the trauma of the implant surgery to the adjacent tooth root, rather than actual damage to the root, which could result in my needing RCT to #12. Especially since I've had two RCTs in my life and both have failed and required extraction - hence this implant - the first of two. I can only assume that my oral surgeon will assume responsibility for the RCT if it becomes necessary.
However, in the meantime, I, as the patient, am the one who is experiencing severe pain, and having to deal with the impacts on my life - like having to eat only soft foods, dealing with antibiotics and their (forgive my candor) attendant side effects for women, and worrying about whether I'm going to have to have yet ANOTHER root canal in a tooth which did not cause me pain until last week - in addition to worrying about whether or not my implant is going to succeed or fail.
I found this forum in searching Google for "pain after dental implant" and the original poster's question is disturbingly close to what appears (on the x-ray this week) to have happened to me. So - how about some compassion for your patients, dentists?
That said, thank you to Drs. Joshi and Wallace, the only two dentists who seem to realize that service to the patient and patient comfort are important considerations. I would urge the rest of you to think a little more of your patient as a person with a life they're trying to live - without pain - not as just a "case."
Richard Hughes DDS, FAAID
9/17/2009
To Recent Implant Patient, You are correct. We docs have to pay attention to detail and care about you the patient(s).