Implant Placed in Inferior Alveolar Canal: Timeline for Patient Recovery?
Dr. D. asks:
I recently installed an implant into the inferior alveolar canal in the #19 area [mandibular left first molar; 36]. Upon realizing what I had done, I backed out the implant and replaced it with a shorter, wider implant that did not penetrate the inferior alveolar canal. The patient has paresthesia in the left lower lip. Should I expect that normal sensation will eventually return? Should I be giving her a steroid to stimulate recovery? What kind of timeline should I present to the patient?
implant in inf alv canal
pre-op
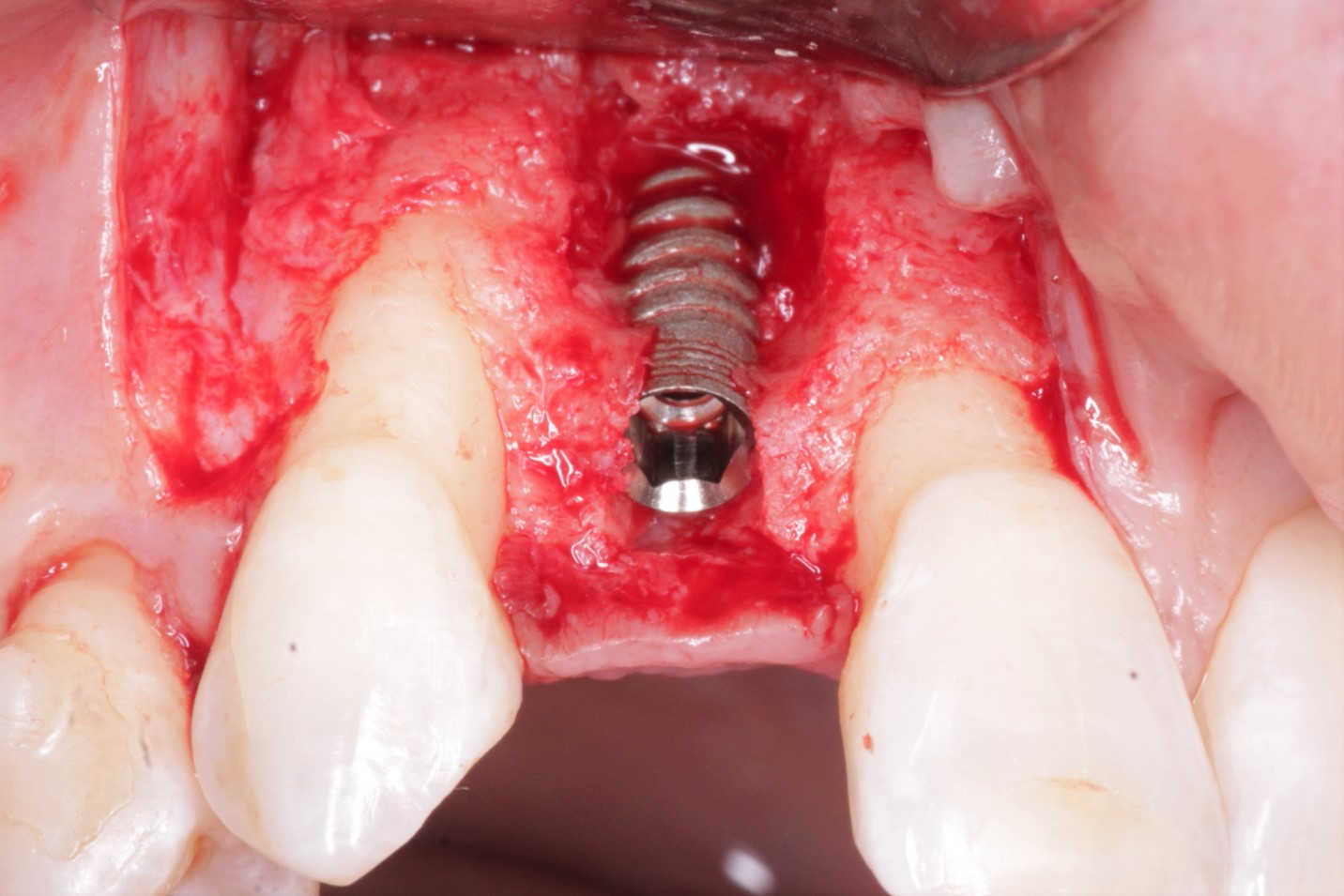
implant changed to shorter and wider 4.3*10mm
during the procedure
77 Comments on Implant Placed in Inferior Alveolar Canal: Timeline for Patient Recovery?
New comments are currently closed for this post.
Leal
1/30/2012
Next time take 20 x-rays if necessary with the smallest diameter bur to check osteotomy length. For now some vitamin B1 prescription will aid in neurogenesis. It could take a while to recover and low intensity laser therapy might be needed.
Good luck.
MD
2/3/2012
The Sensation has recovered.I think it was only the pressure from the 13 mm implant which had caused the parasthesia.Thanks for the response.
Dr. Alex Zavyalov
1/30/2012
Not always one implant can adequately substitute one missing tooth. In this case the span is rather long and prosthetic component will be questionable.
eric
1/31/2012
Does look like two implants and two bicuspid size teeth, to fill the span is what is needed. Instead one was placed in the middle, and a tooth that large is biomechanically unfavorable.
Dr L
1/31/2012
I really appreciate this website to allow practioners to ask and answer any questions we have. Unfortunately i feel youre going to cop a fair bit of criticism for not knowing how to handle this case. Try to ignore it. There are a number of similar cases/scenarios on this website that will help you.
Im relatively new to surgical placement of implants, but i have to ask- you took a number of radiographs during the procedure to check your osteotomy (which is good) but one of the radiographs shows the prep drill to be in, or at least very close to the inf alv canal. Did you change any of your planning after seeing this?
DR MILIND DESAI
1/31/2012
In the given OPG the 3.8 mm 13 mm long implant is 2.5 mm subcrestal.So long as the implant was equicrestal It was having safe distance from the inferior canal.When I tried to remove the implant to make the distance safer from the anatomical landmark by turning the implant anticloclockwise..may be because the osteotomy was wider than the size of the implant..i could not get the implant up....because of the verical pressure to engage the implant, the implant went further down.The quality of the bone was not very dense.(h/o extraction 6 months back).No anticlockwise motion was helping me to recover the imp[lant.Finally I had to use currette to lift the implant up.After the 3.8 implant was removed I had not to use any twist drill to place the 4.3 mm implant.I just used the osteotome of 4.3 (having realized the poor quality of bone) and placed 4.3 mm implant with good primary stability.
David Sanchez, DDS
1/31/2012
Suggest not to consider implants over 12mm in posterior. If width allowed a 5mm x 10mm would have been the correct choice
MD
2/3/2012
When I realized the proximity of canal I tried to unscrew the implant .It was not gettinng unscrewed due to wider osteotomy.i had to lift it with currette.Then I used only osteotome to widen osteotomy to 4.3 mm and placed another 10 mm implant with good primary stability.The sensation is recovered now.Thanks for the response.
Juan Rumeu
2/8/2012
There is a big diference in prognosis if you have drilled down 13 mm and placed 13 mm implant or you have drilled down 10 mm and then placed a 13mm implant. The prognosis is rather different: if you have drilled 13 mm the nerve will never recover. If you have drilled 10mm and placed a 13 mm implant, the nerve has been injured by pressure, so it will recover between six months and one year most probably. we learn from our mistakes, and it is really recommended to place implants on the lower jaw ALWAYS with a cone beam tac scan and go the safe way. cheers.
Dr.Alexandru BURCEA, DMD,
1/31/2012
you can prescribe ALANERV.is very good in nerve recovery after injury.sometimes it works.....depending how much you injury the nerv.
sergio
1/31/2012
You might as well suggest taking vitamin to patients with nerve injuries. The supplement ( yes, I call it a supplement, not medication ) has description of some fancy vitamin at best from what I've researched. come on! Let's be doctors here!
What's a dentist recommending supplements for helping cure nerve damage for? Neuropraxia is nuropraxia if it happens. Sometimes it gets better if you didn't shredd into mylein sheath and everything else with drilling. WHy would you recommend supplements to patients for this not-so-subtle complication?
If this is something that really works, I must have heard about it as revolutionary breakthrough to cure all neuropathy and any form of neuropraxia.
Let's be responsible here!!
MD
2/3/2012
The sensation recovered in 8 days after changing the implant.The pt was on steroids.Thanks for response.
Dr. B
1/31/2012
For future reference, when you are drilling and you suspect that you're getting close to the nerve you should start to feel increased resistance to your drill which means that you have reached the superior wall of the canal's cortical bone. That should be a clue to stop apical pressure, otherwise you will penetrate the canal. This could have been prevented by taking multiple radiographs with direction indicators. I also don't like the second implant you placed. It's too short and not deep enough. Unfortunately the paresthesia may be permanent. Be prepared for that. In other words I would report this to my liability insurance carrier just in case.
sergio
1/31/2012
Steroid isn't going to do sh*t if you already damaged the nerve and worse yet shredded it. I agree with above comment. Contact your malpractice carrier and let them know.
Next time, try to go with a bit shorter implants when questionable on a film. If you are going to use two pice implants, you will wait for integration to occurr anyway. You don't have to force yourself to go for longest implant you can find. If width of the ridge allows, bicon shorty of any other short implants will work. Good luck.
Dr.Alexandru BURCEA, DMD,
1/31/2012
alfa-Lipoic acid
Acid linoleic
Vit E
Vit B5
Vit B6
Vit B2
Vit B1
Seleniu
those are the components of ALANERV and i said the same thing about injury the nerve!and the best for all is to use CBCT and not a simple xray even for easy cases like this one wich was bad managed from the begining in my opinion.look closer on the bone in both parts.
Dr G
1/31/2012
1.This site wasn't implantable in the first place and should have been grafted before. Severe lack of bone formation obvious on OPG. You placed your implants more or less in connective tissue.
2. Implant too long
3. Implant too narrow
4.Implant placed subcrestal
5. Patient's interest wasn't put first, due to rushed treatment
Very poor job, very poor result.
Need to educate yourself more about implants.
JIM
1/31/2012
Stop with the judging bull shit greater than God attitute. The guy had the balls to post here. That's the problem, people cannot ask for help so they continue in their little world. Let's all try to help eachother. We all care about the patient as first priority but dentistry is not 100 predictable. If it wa, robots would be doing it. Lighten up and stop being a d---!
JIM
1/31/2012
100%.......before you get on me....also WAS......typos!
Michael H
1/31/2012
+1000, let's try to help this doctor even if just telling him to go to his liability insurance carrier. You don't have to tell him to plan better next time because he will. Wouldn't you?
JIM
1/31/2012
I agree but Dr. G needs to back off. It's people like him that ruin our profession. He is the type that will throw the other guy under the bus when a patient comes to him for a second opinion. We don't need guys like that in our field. I am sure he has never mmade a mistake from freshman year in dental school. Tools like this guy should be bagging groceries. Sorry, but it really pisses me off!
Sok Chea
1/31/2012
No one is perfect! Right? Dr. Jim. Please try to find solution for him.
I think he is waiting for your help. Please share your experience rather then your criticism. the world will look more beautiful.
Jeff Bueno
3/6/2012
I came across this reply on this post I felt bad for Dr. G. Why would someone post an answer like this? It helps no one and only makes him sound like a verbal bully. Why would someone do that in a place that most dentists use to help each other learn? I have my suspicions.
Paolo Rossetti Milano
1/31/2012
Although the radiological overlap of the implant with the canal does not necessarily mean that there is a contact (think 3D), in everyday surgery it is advisable to keep a safety "radiological distance" from the nerve of at least 2mm.
Having that said, you have hit the nerve and caused a nervous damage. Estimating the seriousness of the damage is difficult if not impossible in the first days after the surgery. Anyway there are some elements that help predict if the prognosis is good (complete recovery) or not (permanent damage):
Are you in front of a slight paresthesia or a complete lack of sensibility?
What is the extention of the cutaneous area involved?
How has the paresthesia evolved in the first days/weeks?
If you think that the prognostic factors are unfavorable, you may want to remove the implant to help the healing.
Time provides the answer, medications are a hope. If some degree of paresthesia is present after 12 month, it is likely that the paresthesia is permanent.
Suggestions for the future:
Make extensive use of intraoperative periapical radiographs.
Use stopper drills.
A CT scan helps.
Also consider that there is the lingual shelf to pay attention to.
Implant therapy is an elective therapy. This kind of mistakes cannot be excused.
Good luck
One question: did you notice abnormal bleeding after you drilled the osteotomy?
DOBS
1/31/2012
Unfortunately in this situation the planning was somewhat less than ideal. A rotary instrument injury (bur) has one of the worst prognosis of any nerve injury. Work done by Dr. Tony Pogrel demonstrated this quite nicely. Vitamins, steroids, NSAIDs had absolutely no impact positive or negative on nerve recovery. Perhaps a referral to a surgeon in your area who does nerve grafts or nerve repairs might be in order.
I used to help my dad around the house as a kid and he always used to say measure twice and cut once when applied to carpentry. It would have been a good lesson in this situation.
Pankaj Narkhede, DDS; MDS
1/31/2012
ALAnerv is not a bad choice as a back up. The regeneration of the nerve will depend on the trauma caused. If u have drilled through the nerve - the nerve is possibly destroyed. If you have compressed the nerve with mild trauma to the nerve the pt may gain sensation 6 - 12 mths?? Diagnose the exact areas of numbness. Hope for the best.
J
1/31/2012
Sergio, strong opinion not evidence based. Let's be doctors like you, uh? There is plenty documentation suggesting that vitamin B can help nerve regeneration, there may not be a solid evidence but still, do you know any better? Like do you use preop antibiotics? Let me tell you, there is no evidence they help either.
Steroids can help relieve the pressure on the nerve cause by the inflammation; that may help, however they have side effects, think seriously before using them.
Vitamin B probably helps in regeneration of myelin sheath. Any side effect? Nope. But we are not Drs like you Sergio. Enlighten us.
sergio
1/31/2012
J, show me the evidence you are talking about vit B helping regeneration of nerve. Basic pharmacology is missing in your talk here. Preop antibiotic tx lacks evidence?
What they do know is once antibiotics gets taken, it's in your blood stream before the surgery. That's more of commom sense if you ackwoledge the fact antibiotics kill bacteria.
Steroid not doing much after nerve injury is also something you should know since paresthesia is NOT cominig from just imflammation of nerve if the nerve has been severed.
Nerve repositioning can cause about 23 to 30 % ( depending on what study you read ) paresthesia itself. Once the nerve gets cut, there isn't much that could be done. Just like muscle tissue, when they get cut, they don't regenerate somehow to reconnect. If you are going to suggest mere vit B is going to do the job, what are you doing on this website? You should be holding conference somewhere with neurosurgeons and orthopedic surgeons about how to regenerate nerve.
J
1/31/2012
Cell Mol Neurobiol. 2008 Nov;28(7):923-31. Epub 2008 Jul 19.
Metabolic and structural role of thiamine in nervous tissues.
Bâ A.
Source
Université de Cocody, UFR Biosciences, 22 BP582, Abidjan 22, Ivory Coast. abdouba3000@hotmail.com
sergio
1/31/2012
J,
Thanks for posting the title.
However, this article merely suggests that thamine deficiency can cause neuropathy ( In more concise way to describe it ) This in no way, suggests vit B can regenerate nerve.
Vit B 12 deficiency could cause neuropathy in diabetic patients as we all know. This is different since it's man made injury.
Not cominig from deficiency of any micronutrient. Gotta have right diagnosis to treat something. Last study that was half way conclusive about the topic was written back in the April of 1994 issue " Journal of neurological science " where ultra high dose of methycobalamine regenerated nervve tissues in an impaired rat. You can't find any conclusive scientific data or follow up article on the topic.
Thanks for the discusion but suggetsing somethng as scientific treatment is one thing and suggesting some out of desperation that are not based on science is another. Best bet is refer this patient to some one better trained and try to get to the truth instead of " Let's try this and that with unproven medication.."
Nerve damage in medically and legally is time sensitive issue for both treating doctors and patients.
Dr. Frederick J. Kapinos
1/31/2012
Get patient into OMFS hands ASAP. There is limited window of opportunity for nerve repair procedures. On east coast the head of Oral Surgery at Mass. General does lingual/IA nerve damage cases:K.Bruce Donoff D.M.D
David Sanchez, DDS
1/31/2012
Suggest not to consider an implant longer than 12mm. The implant of choice if width allows would be 5mm x 10mm
Dr Sujit
12/1/2016
Considering the space between 2nd premolar & 2nd molar, two 3.5 size implants with a single crown over it will be ideal.
Dr. W
1/31/2012
There is an Oral Surgeon in Atlanta named Dr. Baghderi that does microsurgery on IAN and gets wonderful results. But time is of the essence. 3 months is the deadline to refer. I've see some of his work and he is amazing.
Dr. W
1/31/2012
Correction on spelling it is Dr. Bagheri. Dr. Shahrokh Bagheri
Dr BJ
1/31/2012
I think that you have an unknown as for the prognosis. Maybe a little more info would help. Do you know the point at which the nerve became violated during the procedure? If the nerve became traumatized due to overextension of the implant into the IAN canal the outcome would be expected to be more favorable than direct trauma from the pilot drill, which would be more favorable than trauma from the osteotomy drill. Each of these event would in general be expected to have a poorer prognosis as the trauma was greater.
I usually utizize using an infiltration anesthetic facial and lingually of the site rather than an IAN block to provide some feedback. I would likely know if I were getting close to the IAN canal b/c the paitient would feel it and let me know. This is no substitute for excellent pre treatment asassment and planning but helps.
Daniel R Sweet
1/31/2012
Dude,
For next time, realize you rarely need an implant longer than 11.5 mm
Also, did you use a block on this case ?? If so, don't. Infiltration is all you need, and the patient will give you feedback. You can use a panorex or PA if you are confident of the situation. Otherwise, get and cone beam 1:1 x-ray , and get out your digital calipers.
gerald rudick
1/31/2012
Dr. Gerald Rudick Montreal, Canada
HOLD ON A MINUTE!!!!!
We need some more information before we condemn this dentist...the situation may not be as bad as he thinks.
1. The panorex with the long narrow or shorter and wider implant clearly shows that the bone in that area has a large radiolucency.....we have not been told if there was an abcess or cyst there previously lots of granulion tissue,,nor why was the natural tooth lost?
2. In preparing the osteotomy, he/she does not mention if there was excessive bleeding when approaching the IDN....if he/she hit the neuorvascular bundle while drilling, he/she certainly would have noticed severe bleeding...so maybe he/she did not hit the nerves or blood vessels!!
3. The buccal and lingual cortical walls must have been fairly thick and of a good quality bone, otherwise both the narrow and wider implants would not have been secured, as the inner cancellous bone is not very dense, and is very porous.
4.Since we are not getting our information from a 3D scan, and we do not have cross sectional slices to study the anatomy, I would hint that the Dr. D drilled in the center of the ridge, and beyond the Mylohyoid line and into the submandibular fossa ......not even touching the canal,but probably just scoring the lingual wall which would run buccal to the fossa...HOWEVER...in a two dimensional plane, it seems that the implant is placed in the canal......it may not be.
5. 25 years ago, I had the same scare......even worse, when placing a press fit Calcitek implant while tapping....the implant disappeared, and the radiograph showed the implant to be lying horizontal in the canal!!!!!
6. Instead of panicing and calling my lawyer and malpractice insurer, I called an expert dentist at Calcitek, who gave me the explanation I wrote in paragraphs 4 # 5.
7. In my frightening case, the expert advised me to take a currette, go between the outer surface of the lingual cortical bone and the gingival tissue, and fish it out........take the same implant, and gently press it back into place....and let it sit for six months.......this was 25 years ago, and that implant is doing very well all these years.
8. The parasthesia may be a result of trauma to the area by way of an inflammatory response in the canal, and not from being roughed up by a drill..
9. Call the patient back on a weekly basis, with a ball point pen or a pin, gently poke the face and draw an area where sensation is lost.....keep doing the same thing week after week, and measuring the pattern by drawing or photographs....this way the extent of the parasthesis can be measured, and if these areas continue to get smaller......sensation is coming back..
10. In future Dr. D, think about rebuilding the bone, and don't let your patients rush you into putting in implants soon after an extraction..
11. The implant may not take, and get sloughed out because the inner cancellous bone is not 100%...but that could change and it may work......it is causing no problems just leave in osseointegrate a while longer.
and yes.... Welcome to the Dental Implant Heart Attack Club!!!
Gerald Rudick dds Montreal
Dr. Vipul G Shukla DDS
1/31/2012
Nicely said Dr. Ruddick. And politely too!
I think you are right, he would have noticed pulsing splurting blood immediately if he had his osteotomy into the IAN canal. Would never have proceded to place the implant at all.
2D Vs. 3D. Let us hope.
Dr Samir Nayyar
2/1/2012
Very nice & humble explanation sir.
David E. Azar
1/31/2012
Hello Dr. D, Just reiterating what a few people have already said. You have only a 3 month window if there is any chance for nerve repair, (if necessary). Therefore you should immediately consult with an Oral Surgeon experienced in this area! Keep in mind that if you only penetrated with the implant and not the drill then the injury may only be a compressive one, but if you penetrated with the drill this is much more serious and can lead to permanent damage, may be partial or complete parasthesia or other neuropathies. I found this article very informative:Iatrogenic Paresthesia in the Third Division
of the Trigeminal Nerve: 12 Years of Clinical Experience. Journal of the Canadian Dental society, March 2005...search for it at google scholar and you should be able to download.
DFCOMS
1/31/2012
It appears that the panoramic film is digital. If so it is possible to measure the distance of the edentulous space, calibrate your image and measure the distance from the crest to the canal. This will help determine the proper length leaving a 2 mm safety zone. If in doubt as others have said get a CBCT for an accurate look. As far as the nerve goes, rotary injuries are bad and the best advice is map the area and degree of neuropathy and compare over a 2 week period giving the patient antiinflammatory meds immediately, ie. Medrol Dos-Pak. You should seriously consider a referral to an OMS who does nerve repairs and contact your liability carrier as your patient will probably not have any trouble finding someone, like some of the previous commentors, to align with her against you legally.
musician
1/31/2012
This was an interesting post and comments. I can see why some got upset at the directness of others and why others were so direct. While this is to be a learning site and not a condemning site, it still is important to urge those that are early in the learning curve to be cautious and not cavalier when placing implants. The case above is a good example of a number of rather obvious mistakes that has placed the patient in a very compromised condition. There are many experienced implant surgeons around throughout the world and before complications like this occur, every dentist should not be afraid of a consult if questions arise. This case in particular shows several serious concerns: placement of an implant without sufficient foundational knowledge to do so, and this also applies to placing an implant into an osteotomy that is so loose as to not even engage the walls of the osteotomy sufficient to reverse the drive and remove the implant. This really should have been obvious as the osteotomy was being performed. As to the depth, this shows that grossly insufficient preplanning and measurements were made both prior to placement and during treatment. Again, there simply is no excuse for not following protocol of accurate measurements before and during surgery along with checking depth via radiographs if unsure. Of course, hopefully, these mistakes will not be made again by this dentist, but that does not help this patient very much does it.
Implantology is not an experiment anymore. The days of that are long gone and I was in at the beginning having been placing and restoring implants since 1982. Please do not EVER make this mistake again. Proceed with caution and sensibility. And for those that charge anyone being critical with running off a dentist from learning, your points are well taken. But you must also consider that in tap-dancing around the issue and being warm and fuzzy you run the risk of not importing the sense of urgency to NEVER doing this to any patient. To the dentist that may be crushed by being criticized, buck up and have some balls or get out of the practice of implantology, for when you do this to somebody, your treatment was worse than a failure of your technique but rather a destruction of someone else's quality of life.
We cannot address the issue adequately without being very pointed about the serious of a mistake like this. This is not a "tear in a sinus membrane", this is the scrambling of the nerves responsible for sensation in 1/2 of this persons lower lip. Responsibility requires much further education before attempting this again. Don't worry, you will learn. But you should have already known this before you ever picked up the drill.
eric
1/31/2012
OMSNIC is the insurance agency that insures many of the OMS and thus had a large data bank of malpractice info. In their risk management seminars, they state that recovery of paresthesia/anesthesia from direct implant trauma has a much poorer prognosis for recovery than a 3rd molar removal type injury. The best thing you can do at this time is refer the patient to a surgeon skilled in microneurosurgical repair for an evaluation. While the clock is ticking your risk of a malpractice claim is rising. Repairs aren't really "successfull" in a sense of return to normal sensation. However the courts view a timely evaluation and potential intervention by a skilled surgeon as you doing all you can for the patient at this point.
Dr. Vipul G Shukla DDS
1/31/2012
Dr D,
First of all, I admire your honesty and courage in posting what obviously looks like a surgical failure case in front of the general dental community. You seem to be handling it well so far. We are all learning from this, and I thank you for sharing.
From the looks of the pan and IOPAs, dense bone apparently has not filled into the site after the extraction, and I am assuming socket preservation was not done at the time.
If you say the implant dropped into the canal space during your attempts to remove it out, then I hope your osteotomy did not violate the IAN space, in which case, there is only compression trauma to the nerve/vascular bundle. Were U trying to engage the corticated bone of the IAN canal wall for primary stability(need a lot of experience for that technique)? Is that why you chose such a long implant? But 3.8 mm diameter for this wide space, seriously? If the nerve was not severed as would happen in a frank osteotomy, then you still have some hope. If tingling starts returning in about 4 weeks, then there is good hope of regeneration, else refer to a competent microsurgeon as everyone is suggesting. How is it now? Completely numb feeling or some tingling numbness?
Even your current choice of 4.3mm diameter for this wide area is too narrow in my opinion. At the very least patient will have wide triangular embrasure spaces around the crown to deal with on a regular basis. From your screen grab, I see the surgery was done on Jan 25th, which was a week ago. If you gave NSAIDs and supplemented with a bit of steroid to reduce inflammation, then the rationale is actually justified as pressure from oedema inside a bony canal often is cause for necrosis of tissue. In this part, then I disagree with Drs above. A few days of prednisone will not hurt. B group vitamins may be a supplement worth considering for about 4-6 weeks.
'If you fail to plan, then plan to fail.'
As DOBS said above, measure twice, cut once. What is done is done, I for one, am hopeful of regeneration if your osteotomy drills and initial implant did not sever the nerve.
Cases like these, I pray.
Pray a lot.
Good Luck!
Baker vinci
1/31/2012
I'm answering the post because the first ten responses didn't . If the patient suffered just a neuropraxia, then recovery is possible. I would have given high dose steroids immediately. This practice is supported by lots of neurosurgical data. If the patient begins to experience pain, refer them to an omfs trained in nerve repair or a neurosurgeon. The way you managed the situation is approriate in my opinion, but this is where your new cbct scanner will "help".. Most neuropraxias heal spontaneously and nerve repair, should be reserved for patients with unrelenting pain only . Make sure your injury diagnosis is correct. Bv
Richard Hughes, DDS, FAAI
1/31/2012
Baker is on the mark!
DOBS
1/31/2012
I do not wish to be a contrarian but sometimes it is necessary to bring the discussion down to its basic level.
1. Did the pilot drill or any of the other drills penetrate the contents of the canal?
2. If the nerve was injured by a rotary instrument - the prognosis is hopeless without a repair. Even with a repair, at best 75 to 80% of pain free function might be expected.
3. Nerve injuries of this nature, if in fact there has been a burr initiated injury to the IAN, do not recover spontaneously.
4. 3 months appears to be the magic number for repair for successful repair.
5 For all of you that have forgotten nerve injury and repair physiology, there is a die back phenomenon to the first major node. Unfortunately for the IAN, this node is intracranial.
6. The case for the use of high dose steroids, even in intracranial injuries, has not been made. Most Neurosurgeons do not use these drugs as their primary management tool and rely on drug induced comas and mannitol to reduce intracranial swelling. There is no evidence that peripheral nerve injuries are helped by steroids.
7. Why cannot general dentists accept the fact that there has been a nerve injury and the management needs to be moved up the skill level line? We all make mistakes and sometimes we need the assistance of individuals that have special skills.
Baker vinci
1/31/2012
Dr. Sweat, what about us poor oral surgeons ,that put our patients to sleep. We don't get the luxury of impailing the 5th cranial nerve or at least the perineurium to help position our implants. "Dude", I'm going to make a bold statement; leaving the neophyte's patients unblocked, is ill-advised, especially for the neophyte. Bv
Ira Bauman
1/31/2012
I would like to address something some of the early posts mentioned. They felt that the space was too big for one implant and required two for proper prosthetic treatment. I realize it's hard to use a caliper on a monitor but it would seem that the space between the contacts of 18 and 20 is roughly the same as the mesiodistal length of 18. I believe a wider and shorter implant here would be adequate. Any thoughts?
dr serge goldmann
1/31/2012
not have time to read all the comments, but it seems that the implant was driven in the canal due to poor bone density, and not overdrilling. it means that the damage is only a compression lesion, and not a cutting of the nerve. it would get back hopefully. try to mark the non-sensitive zone with a pen and make a photo, and do it every 1-2 weeks, you'll probably see the improvement by diminution of your insensitive zone. if it's the case, even if it will takes time, it will recover.
for anesthesia before implantation in this zone, i do not make a block, but an external infiltration,trying not to involve the mental foramen. if the lip is awake during the surgery (very difficult in this specific case) i'm very safe. even not, the remainig sensitivity of the nerve gives me a helpful alarm before eventually causing any damage.
hoping it helps you- good luck
naser
2/1/2012
Although the radiograph shows the implant is in the canal its not necessarly that the nerve is damaged some times overlap happens
some points to consider next implants
1-at least 2mm distance should remaim between the canal and the implant
2-when u reach the compact bone of the alveolar canal u feel the risistance
3-even if u just penetrated the canal the pt. will feel the pain and tell u .that for this reason we dont give block anaesthesia
and finally good u retreated the implant and backed off .i wish the parasthesia is transient and not permenant .
good wishes
dr.naser. palestine
Baker vinci
2/1/2012
One suggestion, that maybe helpful for future cases is; when removing the tooth and grafting , measure the distance between the most exposed aspect of the tooth and it's apices and this will give you a general idea of how long your implant might be. Disregard any suggestion of maximum lengths of mandibular implants . I have placed 16 mm implants in the posterior mandible. Have you done brush stroke or two point discrim. test? Is the patient anesthetic? Most importantly is she in pain. Be careful in discriminating pain from return of sensation . There is a new, " golden hour", by which to address these issues and it apparently has gone from 6 mos to 3 mos.. It never hurts to seek help from a colleque early on, so that a baseline can be established there. I have personally had one of these, that resolved, on a close family friend. Bv
peter fairbairn
2/1/2012
My 2 cents , Prevention is better than cure here obviously , so always assume you do not know and check constantly with PAs , even with a scan never assume you know .
Serge is correct and this is due to placement with handpieces at a set torque and agrresive implant cutting edges into soft bone ,hence the implant was placed too deep. I always place by hand , lust an old habit .
But the correct procedure was followed post the incident and agree with BV on Steroids.
As I do not think this was a pilot bur type injury , ( although no evidence from the poster ) ther should be a reasonable chance of recovery .
Map the lip for sensation points and photograph , then re-do it a fortnight later to evaluated improvement .
And yes seek help .
Peter
peter fairbairn
2/1/2012
Although I had a laugh about "lust an old habit ", it should be "just"
Peter
Richard Hughes, DDS, FAAI
2/1/2012
Baker, you are correct, when in doub, graft the site, then place the implant. Measure, measure and measure again. Prevention is the best policy.
José Ferreira
2/1/2012
Well, You should have a CT before doing what you have done... At this time, and Knowing that the mandibular canal is placed in a lingual position at the level of the first molar, I would ask a CT to see the damage caused.
I would ask for help to a bioengeneer. There are some improvements in nerve regeneration using a guide tube. Otherwise, you will have a fibrosis that will impare axonal growth and the patient will not have a full recovery.
Dr. Alex Zavyalov
2/1/2012
After reading all 50 responses (it took no more than 2 min) I’ve made a deduce that some of you do not understand that in spite of a full future recovery this is not a prosthetically driven case. It’ll fail because of inadequate implant support.
DrO
2/1/2012
Good post and excellent commentary. I enjoy this site. Thank you all for your input.
DREAM DDS
2/1/2012
Dr. D: Thank you for sharing this case with us. Although there are many very experienced doctors here, there are most likely more who come here that are in early learning curves of implantology. You have heard many valid comments and philosophies that we, as GP's, have dealt with throughout the implantology era. Specialists have issues too, but they have a thought process that backs up their treatment decisions. My comments are for you to consider , did you do these steps:
1. why was tooth removed, who removed it, curetted a lesion?, bone grafted or not? How long was healing? Medical Hx.
2. The appearance of the site is not "normal" post op to extraction.
3. CBCT is now consider standard of care and should be in all teaching courses for implantology. There are some teaching courses, very famous ones, that do not mandate CT in every case, but I feel it is mandantory. This would answer ALL questions needed:bone volume, density, nerve canal. Need for pre-grafting.
4. Mounted pre-op casts for diagnostic wax up of final tooth/teeth.
this will determine the implant size appropriate to carry the occlusal load. You may have seen that two teeth of bicuspid size would be better. To have it in a wax up will educate patient to the treatment.
A radiographic guide is made for the CT or at least, a model based surgical guide with CT to orient the drill angle. A guided
5. All these things will show the "thought process" that is needed for presenting a case and carrying out successful treatment. If your treatment is questioned by a subsequent treating dentist or an attorney, the "thought process" is what will show you had sound basis for the treatment. It needs to be written in record.
6. The one and most important issue you did not mention: Your Consent Form: Did the patient sign a form that stated: dental implant treatment is not guarunteed. There is possibility of infection, bruising,numbness( CAN BE PERMANENT) and loss of the implant and restoration. If you have this document, eventhough your case has a lot to be desired, you most likely will not be found guilty of malpractice.
7. What was/is your formal basic and surgical implant program?
8. Whether it is right or wrong: the fact is that an attorney's first question will be: Doctor did you take a pre-operative CT? and Doctor did you provide the patient with a document of possible complications that included nerve damage and numbness and the consequences of such. If you have these two issues covered, you will most likely be ok from liability. If you don't have these documents, you have very little defense in litigation and the carrier will settle. Are you in US?
9. I must say that I have had many difficult times over my career and that we as dentists have no corner on the holier than though market, we are as exposed to pressures and criticisms and how we react will define us as people. Good Luck
Leonard
Mario Marcone
2/1/2012
Many good comments have been made in response to this case.
I have some concerns.
First, I hope that the effects of this event are reversible, and that the patient is not compromised permanently.
Second, I hope that our colleague has a good rapport with the patient; nevertheless, this may very likely lead to a lawsuit and I hope that our colleague will be able to handle the personal trauma.
I do realize that accidents can happen to us all, and nobody on this forum can really deny that fact.
I am cognizant of the fact that there is a learning curve with everything we do in dentistry--in our "practice".
In implantology, in 2012, whatever we do, it will be judged by the current accepted standards of care, fortunately and unfortunately.
In 2012, implant therapy is no longer an experiment. In other words, if a practitioner engages in rendering implant therapy to a patient, the assumption is that he or she have up-to-date knowledge, expertise, and an acceptable blueprint of thought processes based on training and continous literature review, adoption of a certain evidence-based school of thought, etc, etc.
In 2012, mistakes like this will be dissected to the fullest extent.
I am not trying to be unkind to our dear colleague, but I do understand the severity of reality today given our ever changing (perhaps worsening) social attitudes, economy, and everything else associated with these.
Realistically, if I were this patient, I would probably see to it that I be compensated for damages rendered--and that is the reality today.
Ladies and gentlemen, dear colleagues, where are we headed?
May God help us all!
Dr Mario Marcone
Montreal, Canada
Richard Hughes, DDS, FAAI
2/2/2012
Bolck and Kent's text has an excellent chapter related to this topic.
Robert Markoff, DDS
2/2/2012
@DreamDDS, re comment #6
Informed consent does not relieve you of financial responsibility for negligence. It certainly helps your case if you have an adequately filled out informed consent form and excellent documentation, but simply having a patient sign a document doesn't prevent them from receiving compensation for a "mistake".
Francisco
2/2/2012
Dentistry is no predictable so we need to help each other. Give to patient Alpha Lipoic Acis 600mg twice daily for three months. There is a good medical evidence that it helps neuropathy.
Robert Markoff, DDS
2/2/2012
I think many here that are recommending some form of medication, i.e. vitamin B12, steroids, etc as a "cure" are giving less than stellar advice. If the paresthesia was caused by a mechanical error, the ONLY possible hope for repair would be surgical intervention and the patient needs to be evaluated by an oral surgeon ASAP. If the patient is reporting any signs of diminishing symptoms, then medication/vitamins would be a harmless adjunct to possible healing. The damage has already been done. Now it's time to follow the proper protocol to possibly reduce the damage and help this patient. By doing that, you will be helping your patient, yourself and your legal defense if this patient decides to pursue things legally.
sergio
2/3/2012
Dr. Markoff,
I couldn't agree more.
Dr Y S REDDY
2/2/2012
this is a real eye opener for all budding implantologists, thanks for the post
RDR
2/2/2012
Please remember that in the future for mand implants distal to mental foramen one can use only buccal infiltration and no IANB. When one is close to the IAN the patient will report a tingling sensation. Then it is time to stop drilling and back off 2-3 mm.
3 D imaging is now basic standard of care.
The return of sensory function will occur but can take up to 1 year and then there may be occasional tingling sensations.
Report to ins. but prognosis is good.
Richard Hughes, DDS, FAAI
2/2/2012
Dream DDS, how on earth can a CBCT be required as the standard of care? The reality is that the majority of doctors placing implants do not possess and do not refer for a CBCT study on a regular basis. This is not to say that it is not a nice tool, it is nice to have when needed. To use a CBCT in every case is overkill. I know of doctors that do not know how to read the results of their CBCT that they have in their offices. I use a CBCT onaprons 2% of my cases. The CBCT is far from ubiquitous, and will stay that way until the cost drops to a level that is realistic. I still palpate, measure and take study models and use common sense!
fawaz
2/3/2012
i think that it is very important problem facing the implantology . Nerobean tablet 3 times daily is recomended and vitaminB comlplex...
dr. bob
2/3/2012
These things can happen to just about any dentist. The lines on the drills can be hard to see or other conditions could result in an osteotomy deeper than that intended. This is a risk of placement of implants, and the comments on how to prevent this are good, but what to do after it occurrs it the question. Was the patient immediately informed and given the option of having a consult with a doctor who is expert in evaluating and caring for such an injury? The wellfare of the patient as well as the liability that the dentist may face should at least be a prime consideration. If the implant surgeon is not expert in this area would the use of steroids and vitamins while several weeks of observation go on, with perhaps no change, be in the best interest of both the patient and the doctor?
Naileshgandhi
2/3/2012
I agree with Richards Hughes opinion. Even for length peri apical is very precise . The length of implant is predecided . Clinical methods and judgment are most important . All other imaging methods are guidance only.
MD
2/3/2012
thanks for the response.The sensation is recovered in 8 days after the second implant placement....the pt was on steroids for 8 days.Thanks for responses.
Dr. Vipul G Shukla DDS
2/3/2012
Hooray! Hooray! Great news! You can tell the patient that dentists all over the world were praying for her lip's innervation!
All's well that ends well. But I'm sure that pan you posted will find it's way to many a lecturer's Powerpoint presentation.
Anyways, I hope you will now wait at least 5-6 months before loading that fixture. Let solid bone fill in apically and let fixture completely osseointegrate, good luck.
K. F. Chow BDS., FDSRCS
2/4/2012
Great news! The lesson is to be super-careful in the lower body of the mandible and not to make the mistake in the first place. For reference, check out these other discussions posted a few years ago where a lot of what was discussed has been covered.
http://www.osseonews.com/pain-after-dental-implant-surgery/
http://www.osseonews.com/persistent-numbness-after-implant-failure/
peter fairbairn
2/6/2012
PetGreat news MD as I said earlier I think you followed the correct protocol post the incident. , did you place with a handpiece or by hand?
Peter
Dr Donato
4/17/2012
Excuse me but de tal implants are for specialist, you have to get prepered., general dentist think is just drill and place a screw, leave implants to specialist
Dr. Mraiwa Nuri
11/16/2012
the canal contain not only nerve but neurovascular bundles so parasthesia could be due to pressure on the nerve from intracanal hematoma (injury to blood vessels) or direct injury to nerve which might be complete or partial.. steroid ok if it is oedema but here it is hematoma so no need.. for nerve injury give vit.Bcomplex help in nerve regeneration. parasthesia in most of the time it will not be permenant but it will take time.
advice for you .... while preparing for fexture site you have to be gentle and you can feel that you are perforating the canal and you have to stop drilling... preoperative radiographic planing is very important step!!