Dr. Nick, My advice is that both implants can be salvaged. The #30 site clearly shows circumferential bone loss due to bacterial by-products from the micro-gap that I am almost 100% sure exists because the abutment screw is loose. Why is it loose? Because the angle of both implants is such that when you tighten one abutment screw, it lifts the other one slightly, so even when you get 30 Ncm torque on #30, you are never going to get a tight seal between crown and implant platform, and all the bacteria in the screw channel eventually find a way to reach bone and start an inflammatory process that causes the bone loss you see now. Splinting is a good technique, if you actually need it, I don't see the need here at all. Splinting adjacent implants in the direct-crown-on-implant technique [UCLA method] requires an extremely good lab that will have extremely passive fit of the cylinders on both implants at the same time, a difficult task when you see that both are angled towards each other.
Here is how I would handle this case:
1) Tell patient that you will try to salvage the #30 implant, and there is a 50/50 chance.
2) Start patient on Amoxicillin or Clindamycin at least a day before exploratory surgery. I would also add Metronidazole to the mix.
3) Under full aseptic technique, access both screw channels, remove composite and then the cotton plugs. Smell each cotton plug. If you smell a necrotic plug on the distal implant, don't be surprised, you have anaerobic bugs that exploded in an unsterile cotton plug and just found the micro-gap to reach your tissue and kept multiplying.
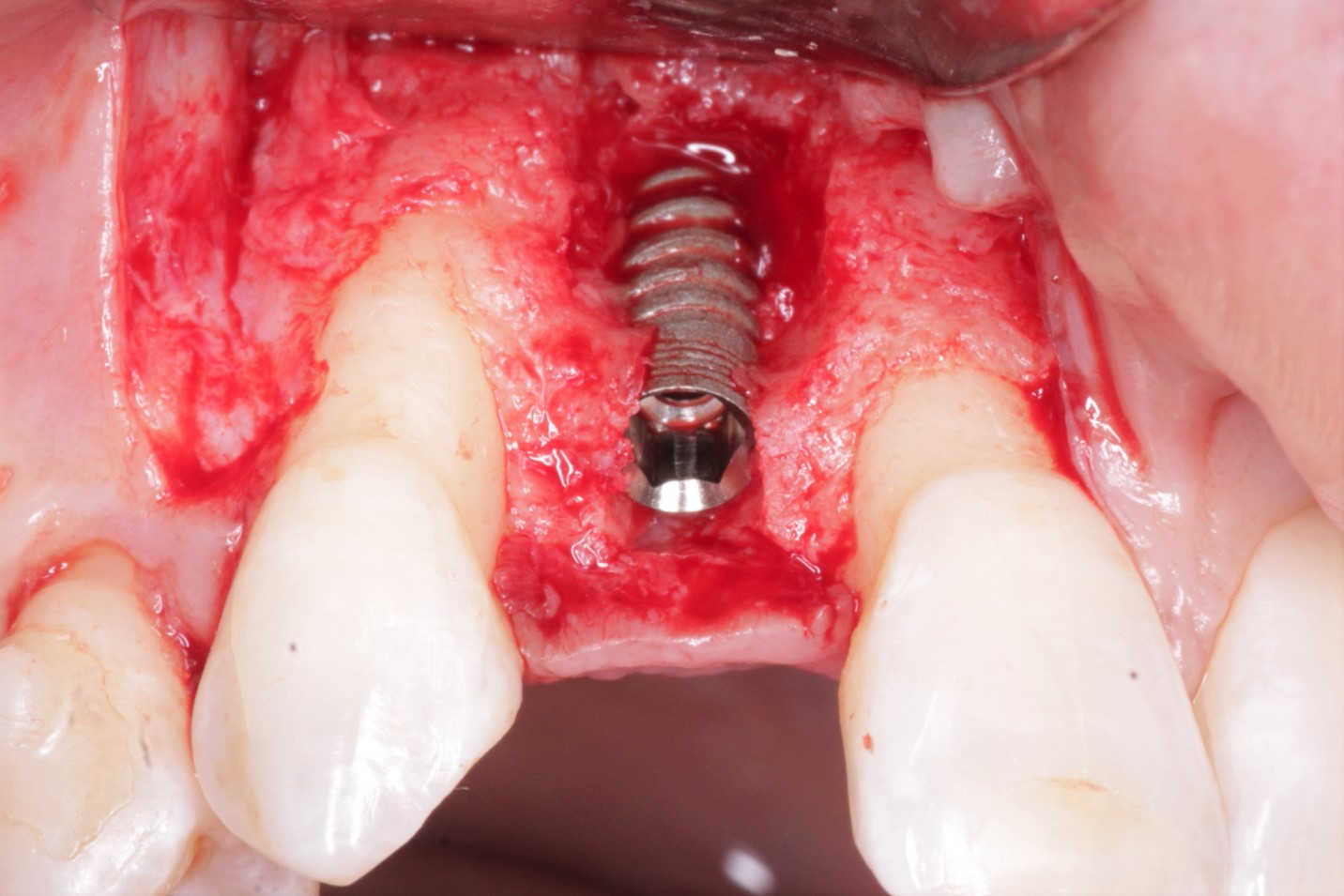
4) Cut away or have lab separate the two crowns such that you can screw back the good crown [use STERILIZED cotton plugs on screw head please].
5) Raise a flap on both sides, visualize the defect, if you only have pus, then it is easier to handle that tenacious granulation that needs to be curetted till your back hurts and you expose fresh bone that bleeds well. You may have to use a round surgical bone bur for this. Make a solution with sterile saline with whatever antibiotic patient is on and flush the area really well. Some people advise to drill out the screw threads, but I feel that a rough surface like Ti-Unite does have advantages for osteoblast propagation.
6) Mix graft with patient's fresh blood or sterile saline and pack the area well. I suggest a graft like Dynablast paste from CITAGENIX (here in Toronto, Canada), which has bone chips in a matrix of growth factors. [osteogenic and osteoinductive potential]
7) Place a sterile healing abutment for the next 2-3 months.
8) Suture tightly around the graft with a sterile teflon suture.
9) Pray
10) CHX rinse for 4 weeks, remove sutures after 10 days. Check-up and X-rays every month, till you see good bone levels high up.
11) Make a fresh crown, and do not splint this time. Use X-ray to make sure that it was seated all the way down. Sterile cotton pellets over screw heads.
12) Have a cold beer and maybe email me if this works out.
nick b
10/24/2013
Wow - that's very comprehensive and clear advice - thank you.
Questions - you suggested making a solution with sterile saline & antibiotic. How does that work please?- i.e how to go through the process & manage the concentration? I will prob have him on Amoxycillin/metronidazole tabs pre op.
Also when preparing/cleaning the implant surface - what technique d you recommend? i.e hand scalers/curettes/ultrasonics etc (I don't have a laser)
thanks!
Vipul G Shukla
10/25/2013
Hello again Dr. Nick,
After the defect is visualised, curette well, this should take at least a good 10 minutes. Meanwhile in a sterile container, dissolve maybe a gram of the amoxicillin capsule content in say about 250 ml saline solution. I have no scientific basis for this, just helping to beef up local concentrations where it is needed most, especially since the patient is on it already. Remember that systemically administered antibiotics can only reach where the blood and plasma circulates, and this necrotic zone has neither, so when you make it bleed afresh and remove the persistent source of bacteria, the body wants to heal anyways, you are just providing the right scaffolding and a little boost with the graft. I have used a sterile endo irrigating syringe filled with this solution and direct a jet at the implant from all sides. Do it till you exhaust the solution you made. If you have a laser, it may help at this juncture, but just gently debriding the surface with a standard titanium scaler should be sufficient, since you mentioned that you don't have a laser.
An ultrasonic is designed to loosen away tartar/calculus, here you will find neither (pus/infection is very acidic), so why add scratches when you don't need any.
Remove the cause/source of the bacteria, and see how quickly the body heals itself.
Good Luck!