Standard of Care for Prescribing Antibiotics After Implant Placement?
Dr. M, a general dentist, asks:
What is the standard of care for prescribing antibiotics after implant placement? If there are no signs of infection at the time of implant placement and the patient is normal and healthy, should I be prescribing antibiotics? If antibiotics are recommended after implant placement, how long is the regimen? Thanks.
9 Comments on Standard of Care for Prescribing Antibiotics After Implant Placement?
New comments are currently closed for this post.
Simon Milbauer
8/10/2010
This is a good question which I ask myself very often too. This was the protocol I was tought at Eastman certificate course to prescribe antibiotics pre-op and then a course after surgery. But, I am less and less keen on that when for example I have a single implant, no grafting, healthy patient, healed site with no history of infections. I have read about also and there are many papers confirming no difference whether antibioitcs have been prescribed or not. Particularly nowadays when so called suberbugs are becoming so common I have really double toughts about it...
Simon Milbauer
Alejandro Berg
8/10/2010
I have to disagree with Dr Milbauer on this. My daddy used to say "if it aint broke dont fix". I have been prescribing antibiotics pre and post op for 16 years and have had great success so why change that. You are still attacking the naked bone if you do a flap and still if you are not making one you will produce hemathome that means poolled blood, nice´playground for bacteria. and that implant deserves the best of thew chances for success.
cheers
Al BDS,FDS(RCS)
8/10/2010
"if it ain't broke don't fix it" is a non argument. In today's practie we are striving for evidence based practises. I agree with dr milbauer on his thinking. I have seen good solid evidence from meta analysis studies describing the increased success of pre-operative antibiotics, but scant evidence for post op.
Dr G John Berne
8/10/2010
Anyone who routinely prescribes antibiotics for elective surgery in uninfected sites is performing malpractice-period!
There are NO indications for routinely prescribing antibiotics in individuals who are not at risk and where there is no active infection. To do so is putting the patient at risk on a number of fronts. Firstly, antibiotic use ,in itself, is not without risk and side effects, some of which may be life threatening. Secondly,the proliferation of antibiotic resistant organisms in the community, and in hospitals, is a direct result of abuse and misuse of antibiotics by the medical profession at large. The problem is of major concern in hospitals,regularly forcing closure of wards following outbreaks of antibiotic resistant infection.
I routinely perform the vast majority of my surgery without antibiotics and my infection rate is as low as anyone's. Care should be taken to ensure the mouth is free of active infection prior to surgery, and use of chemotherapeutic mouthrinse immediately prior to surgery is advised. There are some individuals who are at additional risk and who require extra care. In particular men with moustaches and beards are an excellent source of infection, and the beards and moustaches need particular care with chlorhexidine cleaning prior to surgery, or better still encourage their removal.
It is no coincidence that the National Heart Foundation has recently modified it's recommendation for prophylactic antibiotic use, reducing the need for cover in most cases.
Let's start being part of the solution and not the problem. Stop routine antibiotic use and be more careful with a sterile surgical approach. There should be no need to do elective surgery (which most implant placement is) in patients who have active infection.
Dr.Lscofield
8/11/2010
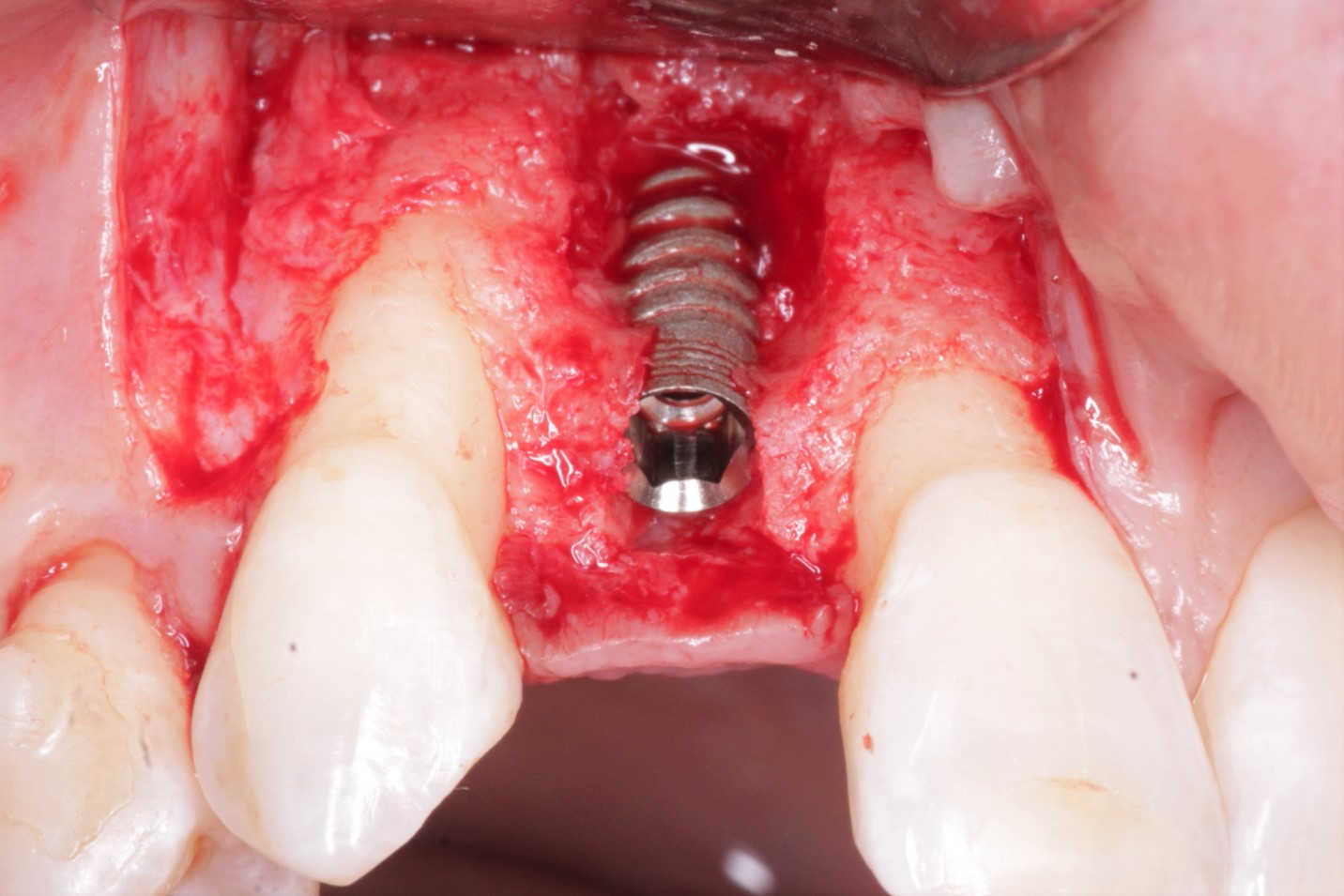
The oral cavity is an infected site, despite the pre op rinse and antibiotic pre medication. Sterile Technique is designed solely to prevent the introduction of any external pathogens. Wearing a sterile surgical gown and gloves, will do nothing against those bacteria living in the gingival sulcus.
The pre op antibiotic therapy, including the Chlorhexedine rinse, which is a local form of antibiotic therapy, will give the patient a few hours of a reduced bacterial oral environment that favors the healing process and helps to avoid a massive systemic bacterial infection.
The post operative antibiotic therapy is designed for those cases where extensive exposure to the oral environment occurs, such as in placing multiple implants or when deep spaces are entered or created, such as in a maxilary sinus augmentation or in a block bone graft procedure. It is also necessary for those patients, who due to sistemic problems, are unnable to effectively fight off infection during the healing phase.
It is a fallacy to extrapolate post op bacterial infection levels from surgery performed on intact epidermis, which is easy to dissenfect and maintain in this state in the post operative healing stages, yet, post op infections do occur in orthopedic implants.
When exposing bone to the oral environment, we enable bacteria to enter the surgical site and the patients defense mechanisms must go to work to eliminate this infection and maintain this state, until the repair process has progressed sufficiently to avoid any furtehr bacterial penetration into the surgical wound.
There are cases where both pre and post operative antibiotic coverage is mandatory and in other cases only the pre op coverage is necessary. In a few ideal cases, the the pre and post op chlorhexedine rinses will be sufficient.
Resnik & Misch give us a plausible regimen for antibiotic coverage, but each clinician must develop his own criteria as to what is appropriate coverage for the specific case of each patient.
Implant Dent. 2008 Jun;17(2):142-50.
Prophylactic antibiotic regimens in oral implantology: rationale and protocol.
Resnik RR, Misch C.
The post operative rinses with Chlorhexedine, rather than systemic antibiotics, provide much better means of controlig the oral microbiota and should be used in all cases, unless there is a specific contraindication, although this article reports it may inhibit tissue repair, based on in vitro fibroblast growth inhibition.
J Periodontol. 1991 Jul;62(7):434-8.
The effect of chlorhexidine treatment of root surfaces on the attachment of human gingival fibroblasts in vitro.
Alleyn CD et al.
Dr. Samir Nayyar
8/12/2010
I agree with Dr.Lscofield
Sanhlabo.
8/12/2010
I prefer pre and post antibacterial regime as infections depends on the balance of the host resistant ,amount of pathogens and the virulence of the pathogens.So,any one going for any kind of surgery,minor or major,will have some form of stress.And stress lower the host resistant.And again,all kinds of bleeding feed bacteria.Causing to multiply more readily for oral pathogens.Oral cavity is already a brutal environment .Who knows the patient will eat or not the kind of dirty foods such as fish paste and pickles?Keep the drugs at base line ,for example,Amoxycilline plus metronidazol,will prevent superbugs.Don't try to jump to superdrugs.
Dr G John Berne
8/12/2010
In response to Dr Scofields comments, I want to clarify the difference between normal oral flora, which are present in healthy mouths, and pathogens, which are the general cause of pathology in the mouth and are the cause of things such as destructive periodontal disease and abscesses.A normal healthy mouth with no pathology present, does not require antibiotics either prior to surgery or following surgery. If pathogens are present with an associated infective process, then I question why you would do an elective surgical procedure before clearing up the infection.
Might I remind everyone of the latest round of antibiotic resistant organisms that are present in the world and posing a potential disaster-the new strain of E-Coli present in Indo-Chinese countries is resistant to most antibiotics and is posing a real threat world-wide.
We are at the cross-roads with antibiotics and if we don't act now we will be back to the days before any antibiotics were discovered,with no available cure for infections. It's now time to use antibiotics appropriately and where indicated only.
Duane Turner
3/19/2011
Is there any current slandered of care regarding the use of ABX. In every surgery care that occurs in operating rooms there is ABX used even in healthy PT. It is not only a slandered of care it is required by the Joint Commission & recommended by The CDC http://www.cdc.gov/HAI/pdfs/toolkits/SSI_toolkit021710SIBT_revised.pdf