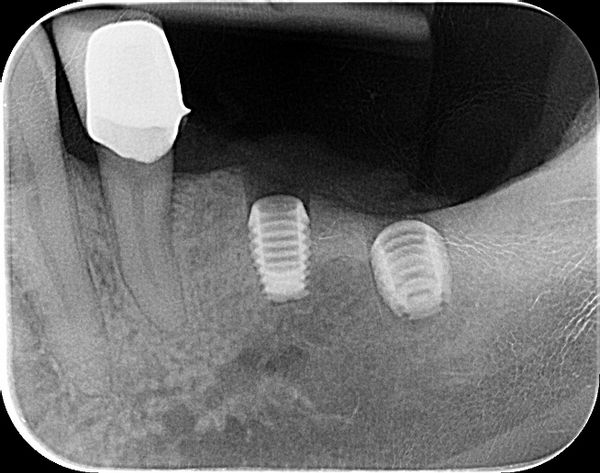
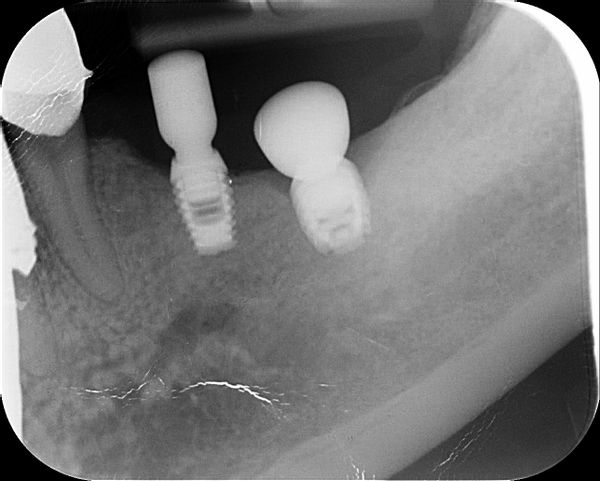
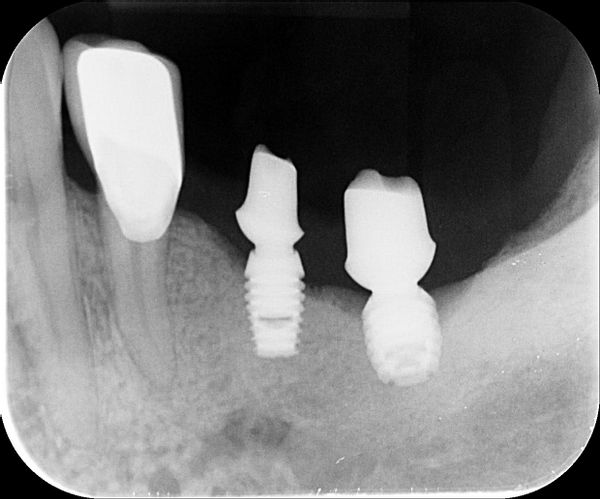
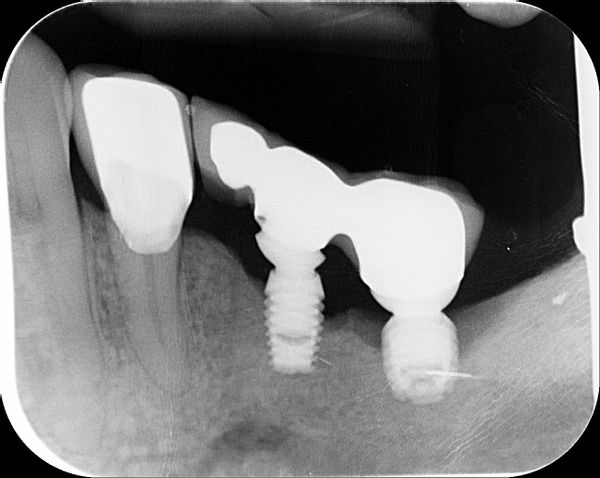
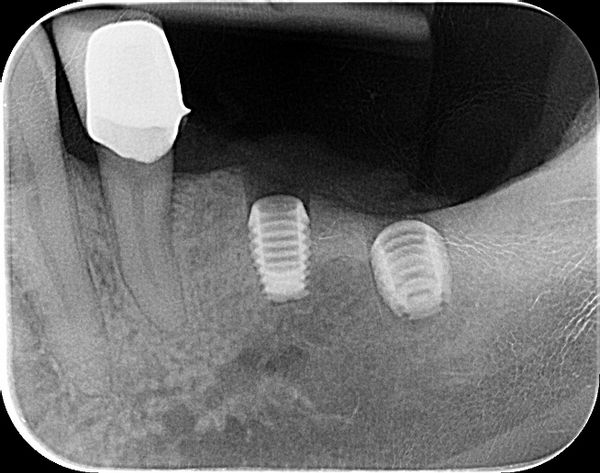
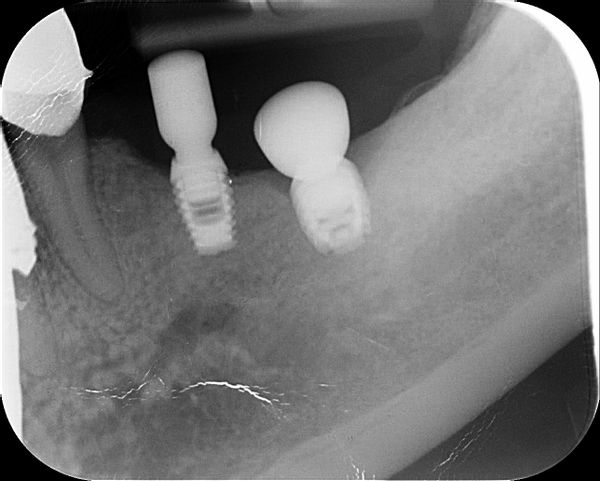
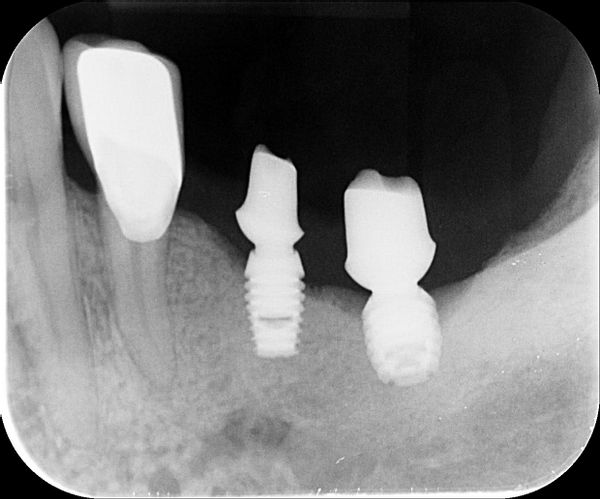
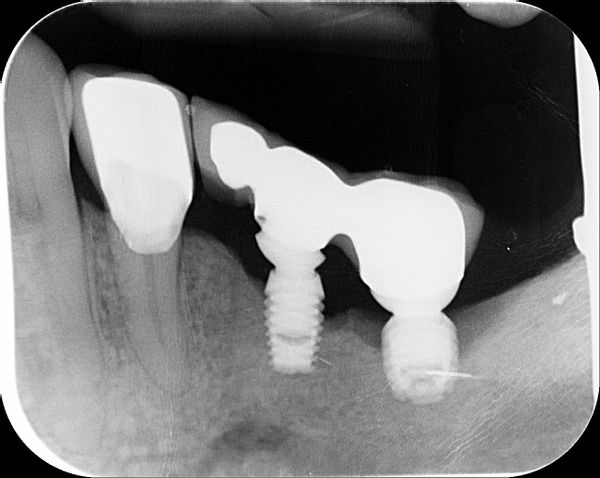
I have placed the Bicon implant subcrestal and some 2 years later I have this. I wonder if I could have your opinions on this case of bone loss around the Bicon implants. The patient has only this side to masticate and there is no contralateral teeth. I know there is heavy occulsion on the implants as well. There was pus as well around the LL6 implant. Why?? Or this just happens? I was thinking of removing the superstructure , clearing by etching the surface , placing Ethoss and then PRF over this and seeing the bone would grow back. It has worked for me before. Or explant and placing again? after Increase in vertical height and then ensure i have bilateral balanced occlusion. Maybe so to signal crowns? so better cleaning. Does anyone else have this?

Nondas comments:
There is very bad fit of the bridge on the abutment of the anterior implant. Did you find cement around the transmoucosal part of the abutment?
MIke comments:
Thank you,
I will take the bridge off and check the fitt.
No cement left.
drv comments:
was the prep done at 50rpm?
drv comments:
Bicon don't use cement or screws, is a tap on
MIke comments:
This patient didn’t want a composite IAC Drv
drv comments:
You can order the Tap on abutments and a bruxir crown, I do that sometimes.
drv comments:
If you want to make a sound decision between fixing or starting all over, best advice is to take a cb scan, so you can see the bone all around. I am guessing this was done without a computer guide.
Andy K comments:
I used Bicon a lot. I think the original problem is that you don’t buried the implant at the beginning. Before you put the crown, there is already bone loss around the implant (9/25/19). I always buried my Bicon and never had any problems with molar area.
Once Bicon get peri-implantitis, it’s hard to deal with, because of its aggressive groves/ design.
If the implants are stable, I would place the black plastic healing cap back, put bone graft and let the implant sleep for 3/4 months.
Finally, in this case, there are too many sub-standard dental works ( RCT/ bridge). The Endo / Perio infections will affect the implants area to some degree. I would ask patient to address the other issues first. If he refuse, I would let him go - to get implants from other office, not mine.
MIke comments:
Thanks Andy,
Ck the first rad, they were both buried and no healing cap on.
Prob I will explain graft and try again and sort out Occulsion.Other areas are sorted now.
The OPG was the start.
doclock comments:
Start with the occlusion after treating bone defect.
Dr. Perdomo comments:
Catastrophic case, I am feeling so sorry for the patient.
Periimplantitis and terrible implant supported restorations.
Completely failed.
MIke comments:
Thank you.
We put out failures on to learn.And seek support from colleagues and guidance so we all learn as is the aim of the forum.
I assume you have never had failure.
They say when you do 300 Bicons a year, it may be only time that some will not behave .normal.
Geoffrey Pullen comments:
I think this is unlikely to be primarily a superstructure fit issue or an occlusal problem. Although Bicon’s can be affected like that, it’s not something that happens in a short space of time.
My conclusion after using Bicon for over 20 years is that sometimes the integration at the crest is not good. Instead of bone forming at that very stressed area, there is granulation tissue.
Be sure to check for this at second stage. If you see any malformed soft tissue there bur it away or remove with electrosurgery.
If you don’t you may have the problem you see now.
Treat these mishaps early. Usually works.
MIke comments:
Thank you Geoff, really useful comments.
Junaid Ahmed comments:
Dr Mike,
It may well be the issue of case selection. If you you used any brand of implant, the likely prognosis may have been the same. A heavily restored and failing dentition, poorly motivated patient is more likely the cause. Your placement of the implants is acceptable as they both are subcrestal as per surgical protocol. Notch it up to experience, don’t do it again . We’ve all learnt the hard way!
MIke comments:
Thank you Junaid for you views.
Shirley comments:
I do agreed with the observation of Junaid Ahmed.
Case selection is the guiding directive, as far as implants are concerned. Presence of infection is likely to contribute to the failure of an implant . Overall assessment of existing conditions is a priority and patient compliance regarding OH is expected. As manifested by various failing restorations, this endeavor was bound to fail , from the beginning. This is one concern that comes to mind, not only in implant placement but other dental procedures , as well.