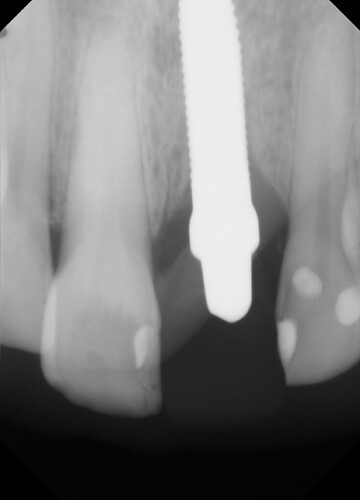
This case presented to me for a restoration of upper left central incisor. Zirconia one-piece implant placed by another dentist and temporized prior. These photos and x-rays are 4 months post operatively. Do you note the gingival inflammation on facial of #9? What do you think of implant position so palatally (the implant is directly inside that lingual buldge of the temporary)? The occlusion is very tight on this case, lowers are hitting directly into the implant. Implant appears to be stable and not mobile but appears to have lost a few threads of bone coverage. Do you think the implant should have been positioned with better angulation? Sorry I don't have cone beam but do you think there is lack of facial bone support based on the periapical radiograph and clinical inflammation?
Mark comments:
Refer this oneTim comments:
I think you are, like many others on this forum, being overly critical of "Another Dentist" or "Another Office" that placed the implant. Is this a good situation for a 1 piece fixture/abutment... No but it is certainly salvageable and straight forward. The inflammation on the facial is most likely cement and if the palatal bulge bothers you then reduce the abutment slightly using a diamond bur with copious irrigation. This is not a problem and "The other Dentist" does not need to be shamed for any reason other than his/her/their decision to use a one piece zirconia based screw despite the overall lack of supporting evidence.Dan Hagi comments:
Having placed and restored thousands of one-piece ceramic implants I have been the "other Dentist" many times before. I can also say that this particular implant has been placed too far palatally, likely because of the thin ridge. This is restorable, however long term may result in tissue recession; as can a two-piece, screw retained implant in the similar position. The only saving grace here is the relatively thick biotype. I routinely place anterior ceramic implants because the tissue reaction is more favourable in thinner biotypes and thus why not in thicker biotypes. The success rates are very much similar with about 3-4% early failures and few late failures that I have seen in the last 10 years of using them. There is supporting evidence though not overwhelming. If you do want to learn more about them ill self promote my online education:Let me know if you have any other questions.
Dr. B comments:
The post was not intended to shame or criticize any dentists, but to discuss the possible challenges of the case and whether the facial inflammation and bone loss at the gingival level is to worry about. And a one piece implant is more challenging because the implant angulation cannot be corrected with the abutment. Besides that I would like to hear thoughts if someone would have done it differently. Like delayed implant placement or guided surgery. It is definetely salveageable, but is it ideal?Bill McFatter comments:
the problem may not be the implant positioning. The dx work up on this case is the problem It is clear that there is a deep bite issue if you look at the restorations of # 8 I suspect # 9 fractured and 8 is close behind This case requires a full workup not just a symptomatic or episodic fix. Unless you can do this and have the patient on board fully with possibly full mouth rehab, then pass on the case Posterior support reestablished-VDO adjusted -anterior support ,guidance and clearance evaluated Lot more here than the placement of a crown on the implantMwjdds,ms comments:
This is restorable by modifying the abutment. However, poor choice of implant and poor decision making on placement. One piece is okay but this then becomes a cemented restoration and should have been placed with the angulation in line with the restoration so there's no cingulum bulge. This implant was placed as if the screw was to exit the cingulum. Implant placers need to understand the final restoration and screw vs. Cement retained before placing the implant.