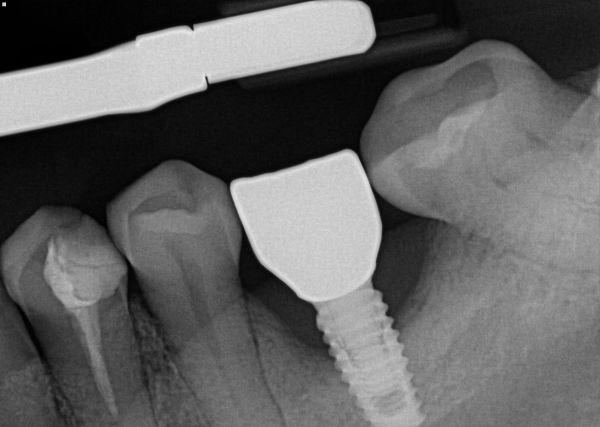
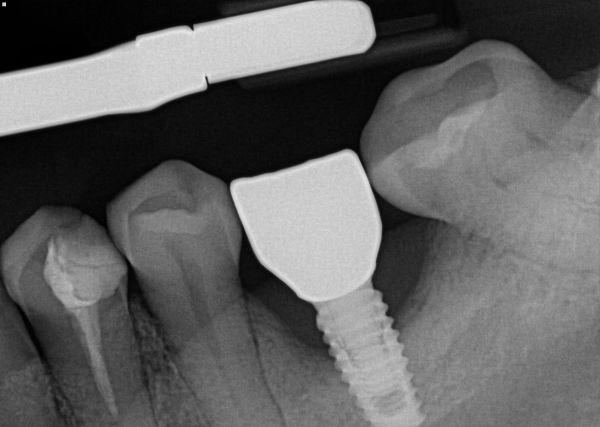
Patient had these implants placed end of 2019 and loaded beginning of 2020. No xrays taken at time of loading. They presented at our clinic with the situation depicted in the images. There was slight inflammation, but no severe bleeding or suppuration noted around 36 implant. What would you do with 36 implant? Monitor, remove crown and graft in an attempt to salvage or remove and restart (or bridge)? Thank you.

Incult comments:
But it kind of is, isn’t it?
Mark comments:
__what is it making you nervous? Not perfect is ok if you inform the patient and monitor.
Can bayrak comments:
The black triangle distal to the crown between the second molar will always remain as an area of food impaction. So grafting may not be a solution
Junaid comments:
If another clinician placed the implant, do not touch it. Whatever happens in the future, it's on your head. Personally, I want to sleep easy at night.
Richard Hughes comments:
If it’s not mobile, take it out of occlusion (unload), detox and graft. Observe
If mobile remove and start over.
Dennis FlanaganDDSMSc comments:
One rule is explant when the probing reaches 6mm
Jerry Schwartz, DDS comments:
Ideally, remove the crown, place cover screw, flap and degranulate....wait 3-6 months and restore with favorable crown and ideal occlusion.
Aquiles comments:
I agree with Mark. It ain’t broke. No mobility. No bleeding. No pain. No problem. Also look at the quality of bone in the area. It looks pretty solid. The chance of getting bone growth to cover this is 50-50 at best. I’m all for use it till it really fails. I’ve seen implants last 10 plus years like this.
Mark comments:
If the patient is 95 years old I would leave it if they are younger I would explain the options and come to a decision together, may be they don't want to go through surgery again. How long will it last in it's current state is very difficult to say, what is the patients hygiene like, I don't see calculus on the rads but their restorative index is high? What is the prognosis for the other teeth that are very heavily restored? You can't treat this in isolation it is in a mouth which is attached to a patient.
As for Junaid's comment about not touching it most of us would have very little work if we didn't deal with failing restorations that we didn't place, this may be more complicated than a broken filling but the patient has come to you for help which should be given either by yourself or by referral. Communication with the patient is key here.
Jeffrey Backer comments:
The other 2 implants look good. So you got to ask yourself, what went wrong? History taking is important. Who did the other 2 implants? Same dr? Goes to evaluating competency. Is there a change in medical status ex: uncontrolled diabetes? Communication is crucial. So many dentists are willing to burn other dentists...I would call whoever did the surgery share the xrays and ask for their input as to why? And document! Put finger pressure on tissue look for suppuration. If there is consider laser detoxification. Or refer. Share the liability if youre lacking the skill set. Rebuilding bone vertically will be tough, success not a given, again skill set assessment. Good luck.