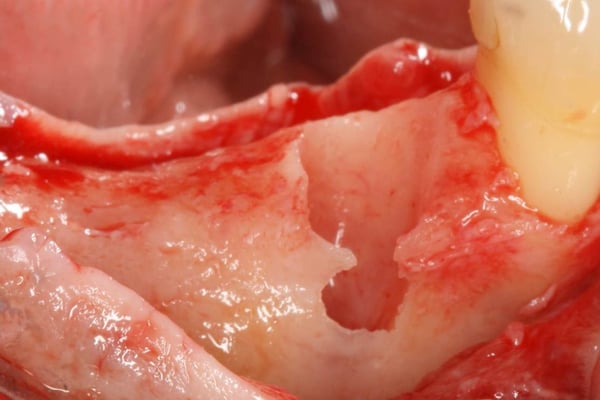
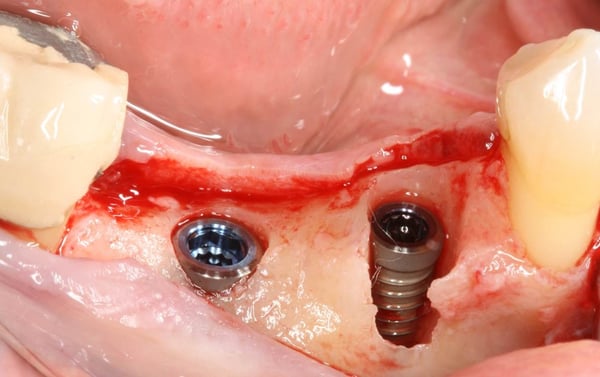
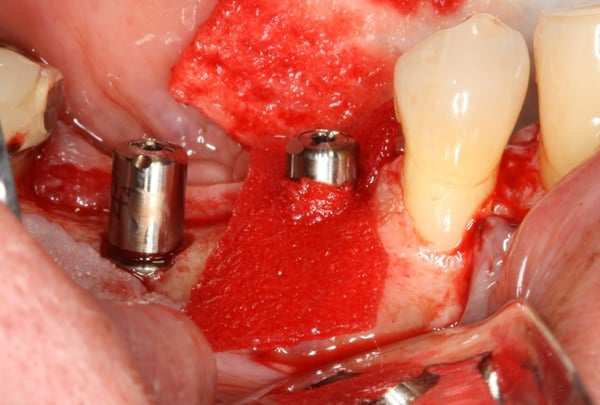
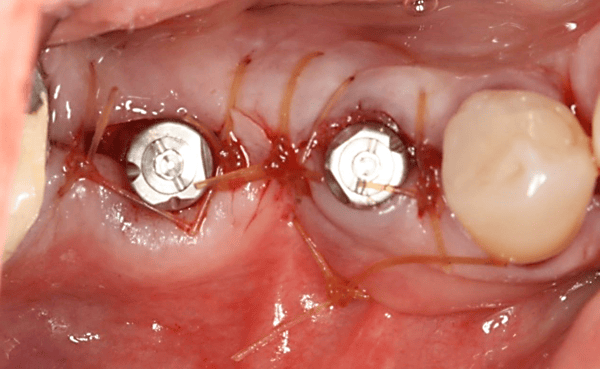
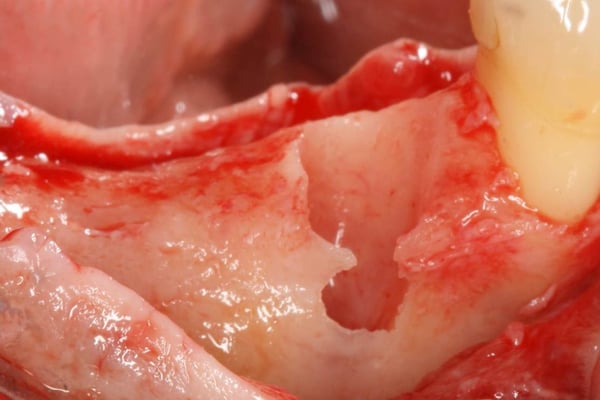
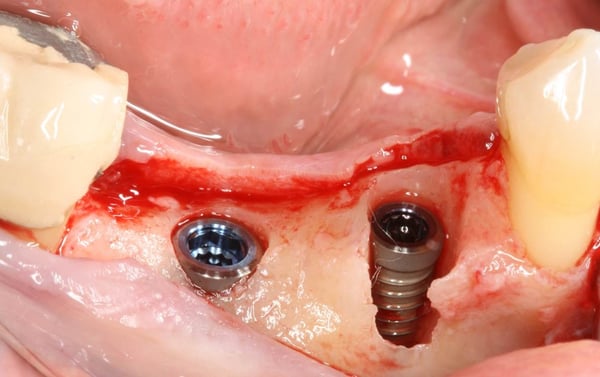
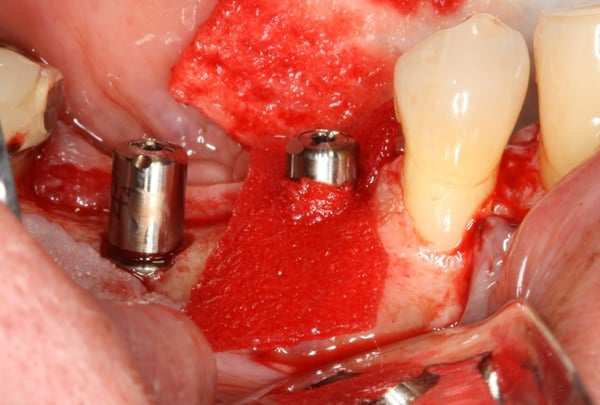
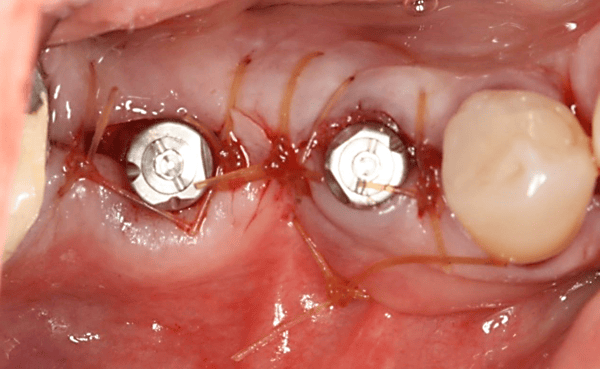
In this video case, Fractured #29 and missing #30 were treated. #29 was extracted and an immediate implant was placed along with an implant in site #30. A challenging (but predictable) bone defect was present at the extraction site which was regenerated using a combination of bone allograft and a resorbable collagen membrane. You will notice in this video that there was a fenestration defect that turned into a dehiscence defect that we need to pay special attention to. But, because the implant is placed well within the alveolar housing we should expect this area to regenerate predictably. Another quick tip you learn in the video is that a good way to stabilize the membrane is to cut a slit at top of the membrane and slide it over the healing abutment.


timcarter comments:
I was taught this technique of popping the membrane over the healing abutment years ago when I was doing my residency in the Army. I still do this though I would argue that it is overkill for this case as the implant is within a 3 walled defect and stabilization of the graft will be adequate without the additional cost of the membrane. Over the years I have observed that contained defects heal very well with excellent bone fill when we allow them too and avoid the temptation to stuff a bunch of stuff in them. Excellent job though and I always appreciate seeing a case performed with quality components and I see you use Biomet 3i along with the Encode. I am a Zimmer TSV guy but I trained with 3i and appreciate when folks stick with quality products despite the industry pressure to resort to cheaper knock off stuff.
drdangober comments:
Thank you for your comments. I appreciate you taking the time to watch the video. I would certainly agree about the predictability of bone fill with self contained defects- we know that well from our studies on periodontal defects. I actually published an article in IJPRD years back about a case of implant healing in an extraction socket without the use of any regenerative materials- you can see it here [https://pubmed.ncbi.nlm.nih.gov/26901307/] if you are interested. In practice, though, I have found that aside from aiming for "bone healing and integration", I also want to achieve contour stabilization/augmentation for improved esthetics and patient comfort which I think is best achieved with the proper materials. Thanks again for your comments!
bromike comments:
if it is a self contained defect, why using a membrane can get better bone contour?
bromike comments:
Without membrane barrier, does it result in the migration of epithelial cells within the grafted site?
timcarter comments:
No. For some reason, in spite of what product manufacturers say, extraction sites even in the absence of an intact buccal plate are still 3 walled defects and thus do not require the use of a membrane. IMHO membranes are way overused in "Socket Preservation" or "Socket Graft" procedures and I attribute this to a combination of aggressive marketing and greed. I can not recall an extraction socket that I have treated either with an immediate implant or with a socket preservation procedure in the past 10+ years where I have utilized a membrane simply because the contained 3 walled defect does not require it. This is my opinion based on 100's of my own cases and while I disagree I will not fault anyone for simply doing what they have been told and continuing to utilize additional and often excessive materials.
drdangober comments:
That is a great question. The way I process this is that there is a difference between defect/socket fill and preservation of buccal contour. I will be the first one to say that these defects will fill with bone without the use of regenerative materials. That being said, changes in the buccal plate do occur which will compromise the ridge contour. So despite achieving fill and osseointegration, there will be a void on the buccal which may compromise the final result functionally or esthetically. I would agree with what *timcarter* mentioned above- standard socket grafting and membrane placement is probably over-utilized. But in my opinion, once a flap is raised and that portion of the blood supply to the buccal plate is compromised (or in this case where the buccal plate is totally missing), a properly used bone graft and membrane can achieve what we want. Thanks again for the question!
drtoast15 comments:
Why did the restorative dentist make such a long contact area occluso-apically?
timcarter comments:
I will attempt to suggest why I think this was done. Look at the placement M-D of #29 and you will see the access hole emerges through the distal fossa. Even though this implant was very well placed it is still slightly distal and thus to avoid a bulbous restoration this was necessary
drdangober comments:
I agree with your analysis- the implant is placed slightly distal which is something to take into account whenever placing immediate implants since the root tends to "dance to the distal" in general and the socket can be misleading. Perhaps another reason the lab fabricated the embrasure this way was to prevent a food trap void due to the lack of interproximal tissue/papilla. Again, appreciate your input.
period comments:
Nice case, well done surgery, good result and very well presented. I to would use a resorbable membrane in a case like this with a buccal bony dehiscence. For the past 2 or 3 years for me this membrane has been an amnion-chorion allograft where I see better and quicker healing compared to a resorbable collagen.
Thanks for sharing your case.
timcarter comments:
Agree this is a great case and appropriate for the intended purpose of this site.
drdangober comments:
Thank you for your comments and appreciate you taking the time to watch the video. I do not have much experience with amnion-chorion membranes but I intend to start using them. Perhaps you can share a little more about your experience with them? Thanks again!
drdangober comments:
Thank you for your kind words. Look forward to sharing more content like this in the future.
period comments:
The amnion-chorion membrane I have been using is Bioxclude from Snoasis. Salvin has a similar membrane that looks good too. I continue to use collagen membranes for larger socket grafts with fully missing buccal bone, ridge augmentations etc. I like the amnion-chorion membrane with smaller grafts over thin buccal bone with implant placement, immediate implants in the open space between buccal gingiva and healing abutment, and sometimes I use them together with collagen or non-resorbable membranes in larger ridge augmentation procedures. I also have on occasion broken a 12 x 12 membrane into small pieces and mixed it in with a particulate allograft and used a collagen membrane over top in a more conventional manner.
The amnion-chorion material does well if small parts are exposed in the mouth, and it seems there is faster gingival regeneration over sockets when using them. I get the feeling there is just generally better healing at the one or two week point when using a-c membranes.
osseonews comments:
Agree with you 100% on the that amnion-chorion membranes are just better all around. Unfortunately, the handling is different than what everyone is used to with collagen, so there is a learning curve of sorts. BTW, both Bioxclude and Salvin A-C membranes are good, but you might also want to take a look at our [DALI Amnion Chorion Membranes](https://www.ddsgadget.com/amnion-chorion-membrane.html).
drdangober comments:
That’s interesting. Can you elaborate on using it by cutting it up and mixing with allograft? Rationale and experience so far? Thanks for sharing!
period comments:
I have used this approach in larger ridge grafts where I am also using another resorbable or non-resorbable membrane over the graft. Here the a-c is chopped into small 2 or 3 mm pieces and mixed with a cortical/cancellous allograft. I have done the same with a small emdogain mixing it into the graft material and placing a collagen membrane over that. The feeling is that the addition of the s-c or emdogain promotes wound healing.
I seem to recall that the a-c material is capable of recruiting stem cells and promoting cell proliferation in healing. It reportedly has anti-inflammatory properties and inhibits bacterial growth.
I have been pleased with early healing and flap repair/closure over the grafted bone. However, I am not basing this on a clinical study showing efficacy.