Dental Implant Micromovement
Dr. C. from asks:
I recently attended a lecture where the idea of “micromovement” of the abutment / implant interface under load not only may lead to abutment screw loosening with some implant designs – but also created a “micropump” of fluid movement that contributed to bone loss. Do certain implant designs predispose to this micromovement? Any Comments on this topic?
16 Comments on Dental Implant Micromovement
New comments are currently closed for this post.
aaa
9/5/2007
Wolff's law applies---where there is movement there is resorption
JW
9/5/2007
I thought Wolff's Law was loading = strength and no loading = resorption. I'm not sure that the "micromovement" concept was around in the late 1800's
Dr. JB
9/5/2007
I happen to know that all implant designs are predisposed to micromovement unless they figure out a way to make the two components (Abutment & Implant) work as one unit to eliminate a chance of micromovement. I did attend a seminar recently in which a specific system did create a bond between two components to make them act as one. I believe they called it the "Ferrule" attachment...I would have to go back to the website to make sure this is the correct name.
The system proved to combine to components together to act as one (like a natural tooth) while it seems other systems out there seem to be trying to make two components work together to minimize micromovement when loaded.
One more thing...I do remember that the system with the ferrule attachment had a friction based system instead of screws which showed to be far superior to the standard screw down systems...it just made sense as to when there is micromovement the best attachment to have is a friction fit because it gets stronger as it is in function. I was relly impressed with the design and asked why this system isn't in every doctors office who places implants.....
DRDEAN
9/5/2007
20 years into this , I have seen micromovement of implant-abutment interface... but cannot prove bone resorption... do I think it happens YEs!..can we predict it ...NO ...but what I have seen and actually looking for on my cases is micro-movement of implant crowns/abutment/fixture as a unit...Where to look? posterior teeth most distal tooh, # 15 or # 2 implant where the contact point opens up after 6-12 months...re appoximated the porcelain to close contact and it opens up again... higher incidence in bone grafted area...How do we prove this??? Don't know...Theory... micro-bone remodeling over time. We know that bone grows and resorbs throughout life...so a 100micron gap is not so surprising in maxillary bone....more things to think about!!!
LC
9/5/2007
Wolff's law is a theory developed by the German Anatomist/Surgeon Julius Wolff (1835-1902) in the 19th century that states that bone in a healthy person or animal will adapt to the loads it is placed under. If loading on a particular bone increases, the bone will remodel itself over time to become stronger to resist that sort of loading. The converse is true as well: if the loading on a bone decreases, the bone will become weaker due to turnover as it is less metabolically costly to maintain and there is no stimulus for continued remodeling that is required to maintain bone mass.
The key of Wolff's law is remodeling and/or load-induced remodeling.
Unfortunately, on site remodeling is impossible for current implant systems. The remodeling process on jaw and surroundings would initiate gaps and may be bone loss as well.
Although micromovement at the implant/abutment interface is not at the bone/implant interfcae, this might be a consequence of remodeling.
Peter Fairbairn
9/6/2007
Maybe micro-movement leads to less bone loss as a result of better stress management?
kemoore
9/6/2007
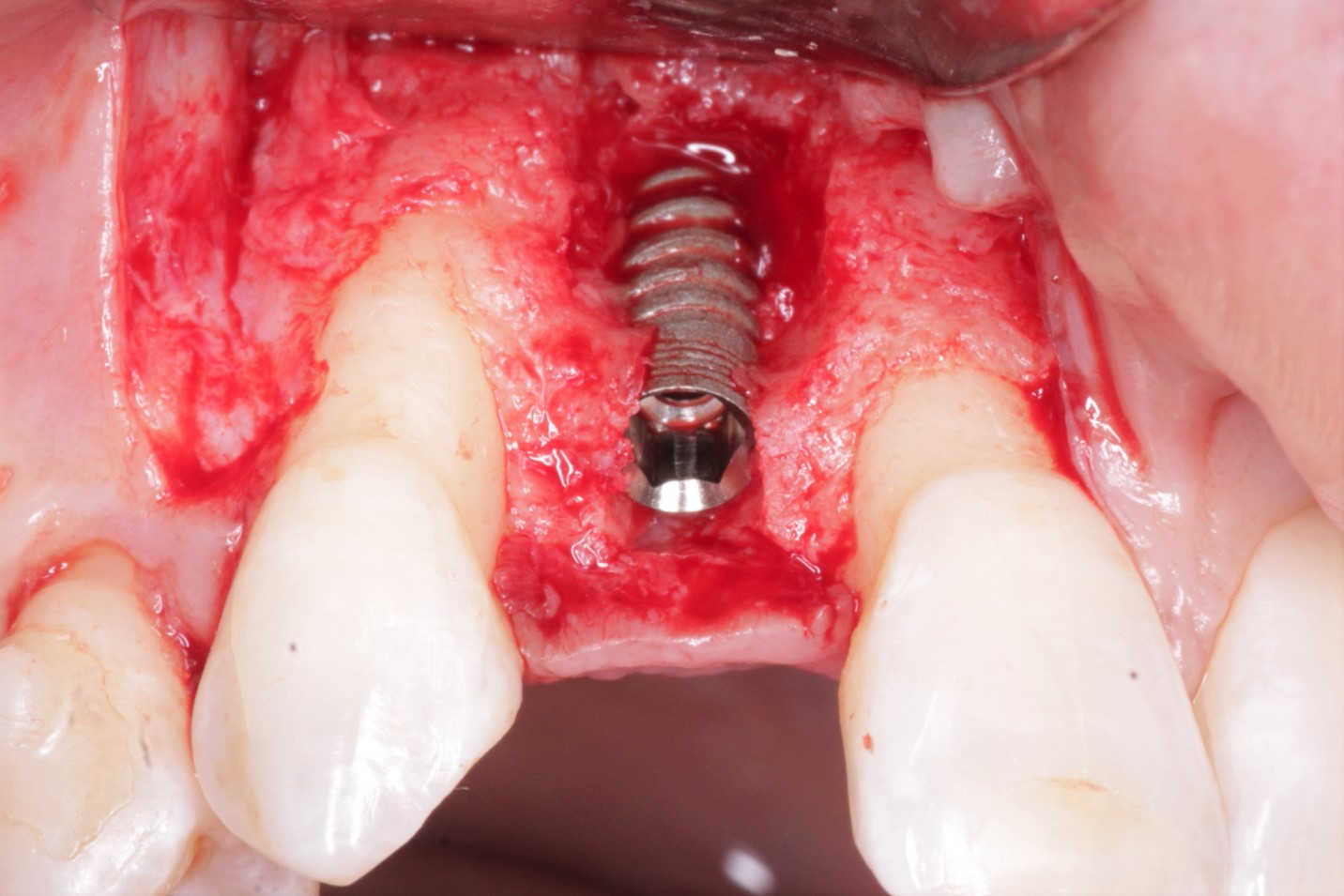
Using X-ray diffraction imaging techniques while applying a lateral load to various abutments, Dr. Weigl at the University of Frankfurt is showing the very real movement that occurs between the implant-abutment interface of various implant systems. This micromovement predisposes to bacterial colonization, and forms a micropump, which pumps bacterial debris and endotoxins into the area surrounding the implant-abutment interface- predisposing to inflammatory changes which result in bone loss around these implants.
Importantly, this microgap and micropump formation is seen with all external hexed systems, and most internal hexed ones as well (and even some with a "morse taper" design).
The most stable result was noted with implants that possess a "Precision-fit" internal morse taper design (there are several of these on the market currently)- this design is such that an essentially "cold weld" is produced when the precision fit tapered abutment is seated to defined torque values (it's not enough to have a morse taper- importantly, it has to be "precision-fit")... this design was the only one (so far) that is resistant to movement and micropump formation...
Importantly, his studies are showing that if there is any potential for movement between the abutment and implant (as is seen with the vast majority of implants on the market currently), then bone loss will result...
dr.amit narang
9/6/2007
i agree with the previous comment that whenever there'll be movement there'll be pumping action and that would lead to influx of bacteria at the implant-bone interface leading to infection.
to overcome these problems only nowadays companies are coming up with two major changes:
PLATFORM SWITCHING
MORSE TAPER
platform switching takes the implant-bone interface away from that influxed fluid,
morse taper reduces the influx,
these two of most important characteristics are present in BICON system, go through their literature, you'll be immensely impressed.
Dr. Mehdi Jafari
9/6/2007
Biomechanics are strictly related to osteogenesis at the implant–bone interface. Controlled micro-motion up to 50 μm at the interface does not impair the process of osseointegration. On the contrary, implant loading might be a key factor in stimulating bone formation. A number of load cycles (daily tooth contact time during biting) of 400 to 800 at a frequency of 1 Hz are expected to have a good cellular response of the bone cells (Kaspar et al. 2002). The loading frequency corresponds to the chewing frequency (1-2 Hz) in humans, so, an appropriate stimulation of the tissue surrounding the implant in the bone would be achieved. As a matter of fact, mechanical stimuli regulate fundamental processes such as cell division and differentiation and determine the tissue type and architecture. This phenomenon is defined as ‘mechanical morphogenesis’ (Benjamin & Hillen 2003). As we all know, loading implants immediately or soon after their placement does not lead but, on the contrary, a certain amount of micro-strain may lead to an improved collagen mineralization at the titanium interface (De Smet et al. 2005; Joos et al. 2005). The strains at the interface, induced by the implant micro-motion, exerts a positive effect on osseointegration, and a 50 μm displacement of the implant seems to fall within the limits of tolerated micro-motion for screw-type implant design. The tissue micro-architecture in the area adjacent to the implant reflects the mechanical micro-environment. Loaded implants display a higher quantity of secondary osteons, whereas unloaded implants are surrounded by more marrow spaces. Adequate force transfer between an implant and the surrounding tissues is essential. Bone stimulation via biomechanical coupling may account for the positive effect of micro-movements on the establishment of osseointegration. However, these micro-movements at the bone–implant interface are tolerated up to a certain threshold and are design and/or surface state dependent.
Dr. JB
9/6/2007
As I mentioned above....the company name was PerioSeal....look into their literature and you will see that it eliminates this possibility and shows great long term results in patients....they also have a screwless system....semi-morse taper with a friction based locking system....go check out thier literature....based on the literature at the meeting and what I have seen this systems proves to work as well if not the best...
Dr. Mehdi Jafari
9/6/2007
Sorry, there is a missing word in the 13th line of my comment and I deeply regret it. The correct sentence is "As we all know, loading implants immediately or soon after their placement does not lead TO DISINTEGRATION AND FIBROUS ENCAPSULATION, but, on the contrary, a certain amount of micro-strain may lead to an improved collagen mineralization at the titanium interface (De Smet et al. 2005; Joos et al. 2005)".Thanks for your attention.
Robert J. Miller
9/8/2007
Getting back to the original question: Does abutment micromovement cause crestal bone loss? Understanding cell and tissue biology gives us our answer. There have been great studies with regard to CFU's (colony forming units)on all of the major implant systems. The presence of bacterial endotoxin results in a proportional cellular response. The production of matrix metalloproteanases (collagenase, gelatinase, elastase, protease)begins a process of tissue turnover. Collagenase, in particular, not only generates collagen fragments that result in soft tissue turnover, but is an osteopromoter of osteoclastic activity and is directly porportional to the severity of periodontal bone loss. THIS is the reason we see crestal bone loss around implants after abutment connection. One piece implants can mitigate this, but you lose your prosthetic options. What we need is a two piece implant that acts as a one piece implant. New abutment designs have brought this microleakage to close to zero; our study will be presented at the AO meeting in Boston next year. RJM
Dr C
9/9/2007
JB, I back from that seminar about 4 months ago, the results were wonderful, I have used the system several times and ease of use is great for the general dentist. There was an article in the last issue of dentisry today. You may want want to look at this. This is the way to go for us generalist
Spartacuspid
9/9/2007
I think JB and C also go by the name of 'Don Callan'....
Don Callan
9/9/2007
Spartacuspid, I am not sure what your comment means. Don Callan
Dr. JB
9/17/2007
Robert Miller is correct is saying, "What we need is a two piece implant that acts as a one piece implant." There are options out there for this and ways to correct this micromovement. We all need to do our research. Research and Science show us the answers. Don't be fooled by the marketing...
Also why limit the microleakage when you can eliminate it...
Now Spartacuspid....my name is Jonathan Bartello not Don Callan....I did hear Dr. Callan speak,, and since then I have done my own research (which I wasn't doing in the past) and I have come across some interesting things about this microvement, microgap, surface area, etc...and when you read the actual studies outside the financed ones by the companies....then you will see a difference in results...Dr. Callan never pushed me in what to use for my practice...He always said it was my choice, however just do your own research to make the best decision...and I did and it is paying off. I am not having the problems I have had in past anymore...PerioSeal has a great product to combat this issue and I will support it until I am proved otherwise..