Fenestration after four months post op: best way to proceed?
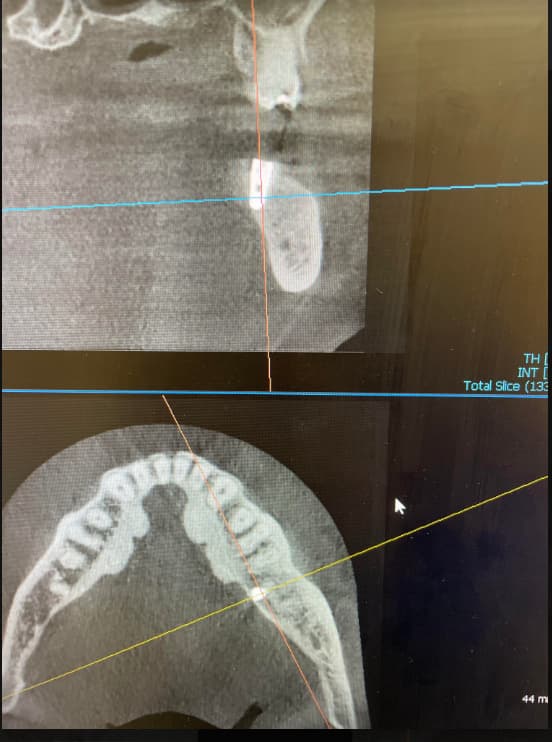
I installed a 3.75mm x 10mm implant in #22 site [mandibuar left canine; 33]. I took CBVT scan before installation and found insufficient bone at apical third ( there was a concavity). So I placed the implant, Mineross and then Bio-Oss over it and then Memlock [resorabable collagen membrane]. After 4 months healing, there is one pin point fenestration in the middle third of the gingiva covering the implant. Slight redness around it. Everywhere else looks fine. I wonder whether i should use just Periowave to decontaminate the fenestration only or go in at the site and decontaminate with hard tissue laser and do bone graft. The opening is quite small, so not sure whether I should open a window like flap there and bone graft. Thoughts?
22 Comments on Fenestration after four months post op: best way to proceed?
New comments are currently closed for this post.
CRS
7/29/2013
Could you get another cone beam or periapical to see if there is a bony defect?
David
7/30/2013
Did you probe the finestration? Do you feel titanium or unresorbed bio_oss? What would you do different this time around that would make the graft successful? Dd you perforate the buccal plate originally? Dd you tack the membrane? The laser is not a magic wand it will only work I'd everything else is done right
Paolo Rossetti
7/30/2013
A "pinpoint fenestration with redness around it"?!?
Isn't it a fistula? If so, there are good chances that the graft has gone.
Perioperry
7/30/2013
Sounds like a failure of the graft, or loss of facial bone from the implant, with bacterial contamination of the titanium and/or of the bone graft particles. I suggest accessing the site via a substantial facial flap (from #20 to #24), debride and irrigate with saline, "decontaminate" the titanium if the facial of the implant is exposed, decorticate, re-graft, tack on a slowly resorbing membrane supported supported like a "tent" with screws, or you could utilize a titanium reinforced non-resorbable membrane. The key is decontamination of the implant. I've read recently of doing this with a laser, but I've not personally had experience with that option. Or, exposed threads can be ground away with a white stone under copious saline irrigation. The AM of surgery start the patient on amoxicillin 500 mg tid for 10 days, PerioGard rinse bid for two weeks.
Vipul Shukla
7/30/2013
A pinpoint exposure right now usually means there is no bone underneath the exposed area for about 3-4 mm at least, if not more. as time goes by and you load the implant, this fenestration might become more pronounced, depending upon the loading angle. This exposure of the implant threads can eventually lead to loss of osseointegration for the entire fixture due to bacterial contamination from the exposed area.
I'm not experienced in lasers, but maybe a semi-lunar flap, decontaminate the implant area, and then graft again, maybe a putty bone matrix type graft, membrane and maybe tack the membrane in this time, and then cover and pray.
Good Luck!
CRS
7/30/2013
Did you ever get some type of X-ray? It would be helpful to determine if the implant is osteo integrated and if there is a bony defect. Grafting bio-OSS over another graft then placing a membrane over that prevents blood from getting to the graft, it could just be the bio-OSS sloughing off under the mucosa. I am unclear if a concavity means a periapical pathology which could be a retrograde peri-implantitis. I feel a diagnosis is required before suggesting treatment.
Peter Fairbairn
7/31/2013
CRS , great to see you write that as I have not used a membrane once in the last 2,000 grafts for that reason , I too feel they are a hinderance to healing not a help.
Raise a site specific flap as to not involve the attached gingiva , Clean Implant with a prophy jet (Tastepe et al JOMI ) a graft with a fully bio-absorbable graft material to encourage real bone which can turn over naturally .
But as CRS says more information would be helpful , diagnosis online is fraught with mis-conceptions.
Regards
Peter
CRS
7/31/2013
Thanks Peter great minds think alike! The only time I use a membrane is if I am concerned about epithelial in growth since the blood supply is compromised especially in a cortical onlay graft. I am moving away from the bovine and porcine products and going with natural human fibrin, human amniotic or Teflon which only stays in temporarily ah a tissue guide to allow guided regeneration. I think the body handles human tissue best for regeneration. But I routinely don't use membranes just a healthy flap with primary closure. For larger more complex grafts then a membrane may be helpful for space maintenance. I am interested in this post since at four months I have seen this complication and it can vary from, non-integration, Periimplantitis, graft loss or simple graft sloughing with an intact integrated implant. I always question when to intervene, regraft, debridement, laser (lapip) or replace the implant. It seems six and fourteen weeks are critical times. Bacteria at implantation surgery or host factors with latent bacteria . Good to hear from you as always.
naser
7/31/2013
fistula arising from implant after 4 monthe s of healing time usually means that the implant is not osseointegrated at all ,check again for mobility and pain on probing ,if so it means no ossiointegration occured at all and u will find that the buccal plate is gone,
i suggest explant ,curret the site properly ,graft and re-implant in 3monthes time
Peter Fairbairn
7/31/2013
As you say many variables , the cases that do not go as planned are the interesting ones . Host response is a critical area in this type of dentistry.
Regards
Peter
Richard Hughes, DDS, FAAI
8/1/2013
Peter and CRS, I strongly agree with both of you. I usually use the barrier by bulk method (increased thickness of particulate and release the flap for primary closure). As both of you know the blood supply comes from the decorticate bone and the periosteum.
My choice of particulate is OsteoGen.
K. F. Chow BDS., FDSRCS
8/1/2013
Yeah. If the implant is not osseointegrated, remove it and replace with a smaller diameter and longer implant...... say 3.0 to 3.2mm diameter and at least 13 to 14mm long. There is usually plenty of bone height here and keep it well away from the labial plate this time. But if the implant is osseointegrated.... raise a full flap, remove the inflamed tissue. The exposed part of the implant should be removed up to 2mm deep away from the labial plate. Yup.. use your high speed diamond round and remove the exposed titanium until there is a decent hollow to place your bone graft with plenty of contact with living bone. Then graft it with with tissue friendly graft based on calcium sulphate and calcium phosphate that can set hard. Close the flap and stitch close all the gaps.
sb oms
8/2/2013
Dr. Chow-
I aggreed with you all the way up until you described removing the exposed portion of the implant.
Would you really let someone do that to you?
Grind the implant into fine dust while a flap is rasied, and then try to graft something that is outside of the alveolar housing?
No Way-
This is a failed implant. It has not even been loaded with a restoration. Whatever your diagnoses may be, it should be removed.
remove, get soft tissue healing, scan, graft, scan, place in solid bone.
K. F. Chow BDS., FDSRCS
8/3/2013
Yeah sb oms. Atomize the unwanted part of the fixture with a precision titanium atomic blaster. Make sure the graft is closely intimated with the peripheral raw bleeding bloody bone. Titanium dust is biocompatible. Drill some holes through the surrounding cortical plate if necessary. If the implant is already osseointegrated, that is what I will do for myself. The alternative is that in removing the osseointegrated implant, there will be a big bony defect which is a prologue for prolonged big procedures that may result in a bigger problem than before. Happy grinding!
Perioperry
8/3/2013
K F Chow puts it coarsly, but in reality this procedure works if the problem is limited to the facial aspect. I've salvaged to similar cases utilizing basically this approach.
CRS
8/6/2013
What is the purpose of implant thread removal ? Removing contaminated surface or to get space for a graft. Will the bone adhere to the naked titanium or a non resorbable bone patch, hard set. Could the surface just be decontaminated with laser or chemical? I've seen thread removal for hygiene in the exposed oral cavity? I just did a case where there was a void it the bone with granulation tissue since the extraction site was not grafted and it was a endo failure. I curetted, used tetracycline and placed cadaver bone. Will wait 12 weeks and pace the implant. Could the bacteria in the bone be the problem? I see this and wonder that if the bacteria and epithelium is removed the graft heals well tells you that it s safe to proceed with the implant. However the cutting of the threads can expose bacteria. Perhaps a technique to truly decontaminate the implant site at extraction or placement. This requires some thinking!
CRS
8/6/2013
P.S. Peter, no membrane!
K. F. Chow BDS., FDSRCS
8/10/2013
Not just the threads...... the implant proper itself. The purpose of removing the exposed surface of the implant at least 2mm deep is to allow a reasonable thickness of bone graft to be placed against the implant as well as intimately with the surface of living bleeding bone. If osseointegration of the implant has already taken place, it should not be removed but grafted where it's nakedness show. Removal makes no sense because it will result in a large defect in the bone that will be difficult to address and will require a bone graft any way. Rehabilitating an already osseointegrated implant is better than to remove it and end up with a bigger challenge! But if it is not osseointegrated, then remove it.
Sb oms
8/3/2013
It makes no sense to me to try and save this implant-
It is by definition a pre-load failure
CRS
8/7/2013
Total judgement call at surgery, I have been burned also in trying to salvage a preloaded implant and have also been successful with salvaging one. That's what I like about wisdom teeth they don't grow back!
Peter Fairbairn
8/12/2013
Hi CRS , yes I use or mix materials that use either CaSO4 or less often a poly-lactide in the graft material so that the material becomes its own membrane as well as more stable through out the graft.
But the difference is it will be vascular porous and this porosity will increase as the CaSo4 absorbs in the first 3-4 weeks .
The key being improved angiogenesis in line with the bodies healing protocol .
Thus no collagen type membrane or autogenous bone to interfere with this healing which may result in improved host response to healing .
We normally load ( Checked by Osstell ) at 10 weeks even where the defect may be both buccal and palatal and the implant is initially held by a thread or two .
Again working with the bodies protocol and utilising functional re-modelling to further assist regeneration .
So I feel the traditional collagen type membrane may be more of a hinderance than a help in bone regeneration .
I have just had another look at Steiner Labs site , great work Greg going in a good direction.
Regards
Peter
peter Fairbairn
8/12/2013
As to this case just check with Osstell or reverse torque to say 50 Nm to check integration if good then clean and re-graft as Dr Chow mentioned .
As to cleaning the surface we feel as was show by a recent Systemic Review by Tastepe et al in JOMI that prophy jet cleaning is best for the surface preparation prior to grafting. Bacteria are everywhere in the mouth , and using bacterio-staic graft materials there is no problem .
Peter