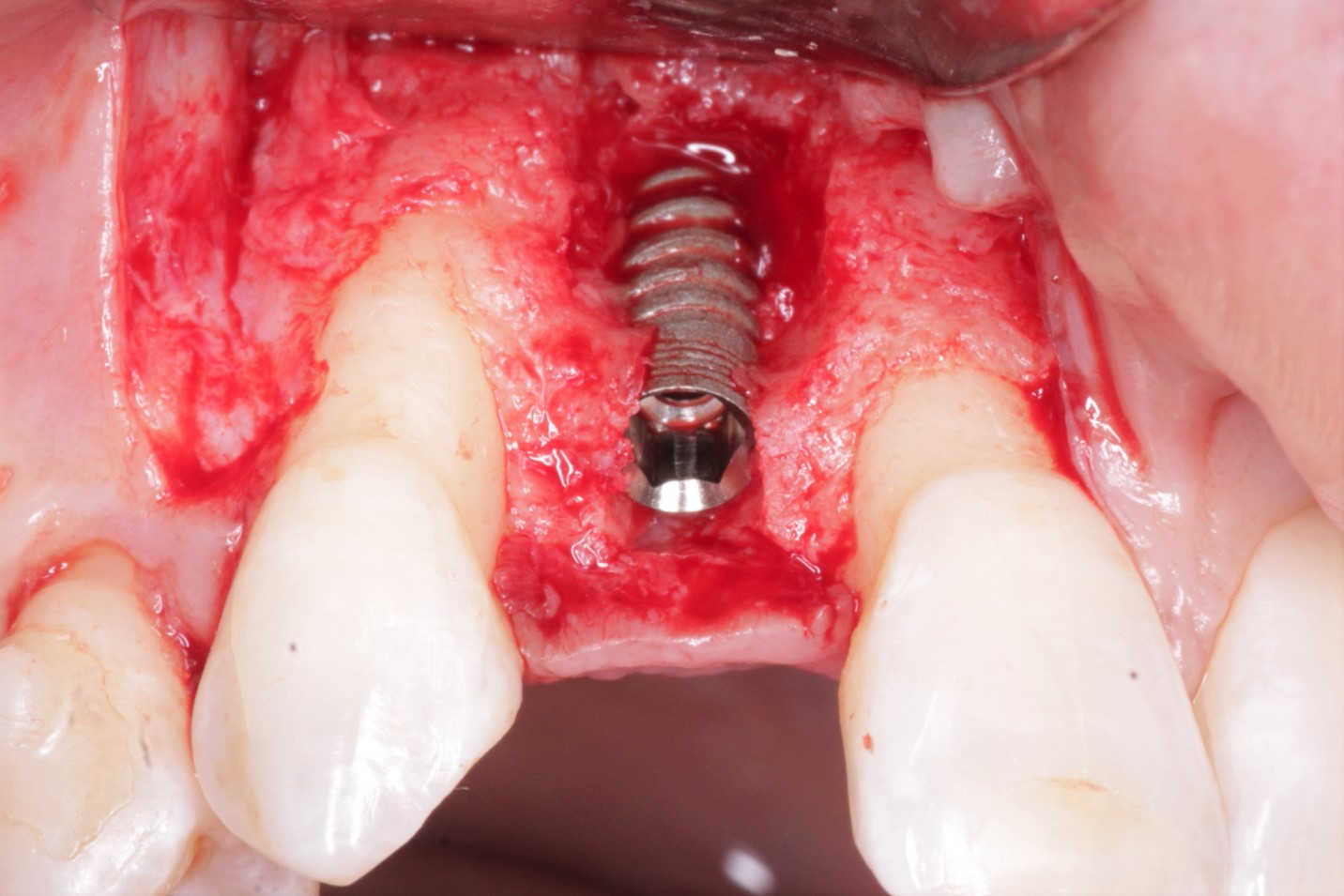
Fractured non-restorable tooth extraction and periapical lesion: advice?
A 69 y.o female patient has a fractured non-restorable tooth #31. CBCT was taken and periapical lesion was noted close to IA canal. My plan is to leave the periapical pathosis and let the body take care of the healing. What if there is minimal bleeding or no bleeding at the extraction site? Would you induce bleeding and curette out as much of the cyst and leave the apical portion? Would you place a collagen membrane or bone graft? How can I prevent fibrous encapsulation of this site? I appreciate any advice on this case.
Thank you

9 Comments on Fractured non-restorable tooth extraction and periapical lesion: advice?
New comments are currently closed for this post.
Dr. Gerald Rudick
10/24/2019
Extract the tooth....look into the socket, and with a fine curette , tease out the broken portion of the root remaining.....gently curette the area, removing the granulomatous tissue, and do place a collagen plug which will aid in the gingival tissues growing over the socket, and will prevent food from getting lodged in this space. Cover the patient with an antibiotic, and necessary medication of pain ……… recall the patient a month later, to make sure that all is well.
Neil Zachs
10/24/2019
I would double check your nerve tracing. It seems like you have multiple lines. If the most superior is accurate, then it seems like there is a thin layer of bone present to the nerve and you should be fine. Currette out infectious tissue as best as possible, to clean bony margins if you can. My guess the site will bleed nicely as the bone has decent marrow spacing. Then place an FDBA graft. If an implant is desired, you would have to keep it shorter anyway to avoid the lingual undercut that is clearly evident on the cross sectional view. Best of luck!!!!
Neil Zachs
Periodontist, Scottsdale AZ
Joel
10/24/2019
I would absolutely atraumatically extract the tooth and remove the pathology. Leaving it in and hoping it will resolve for me is not an option, from what I can see from this x-ray, there appears to be bone between the lesion and the IAN so affecting it with careful enucleation should not be an issue. I always suggest a socket graft with allograft. It gives the patient more options for the future, enhances the healing and costs can be adjusted for the benefit of the patient if they feel future treatment will not be needed. I cover all socket grafts with a PTFE membrane, sutured in place. I typically just curette the socket and not initiate a lot of trauma for bleeding. These site almost alway heal great.
Dr. Moe
10/24/2019
Hi Joel,
Quick question, for a survey that I am doing in my head about PTFE membranes, Do you try to get primary closure every time with PTFE membrane, or do you leave soft tissue open to allow Keratinized tissue to grow over?
Thanks in advance.
Carlos Boudet, DDS DICOI
10/24/2019
Can't read the scan well with such a small image but It looks like there could be lesions on adjacent teeth/areas. Follow the advice given in the previous comments. We all agree that carefully curetting the extraction socket and grafting is indicated. Cover with antibiotic and follow the patient's healing.
Good luck!
Robert Horowitz
10/24/2019
Extraction and debridement are a must. The longer you wait to graft or barrier protect the site the more horizontal and vertical collapse you will obtain as all literature shows. If you can't predictably remove all of the apical granulation tissue, an Er:YAG can sterilize the residual material there.
Sajjad A. Khan DDS,BDS.
10/24/2019
Make life simple and safe > Ext carefully ,remove the PAP then let the surgical site heal 4 to 6 weeks then graft then later insert implant .
Ed Dergosits
10/25/2019
Why so many procedures? Personally I would extract the tooth and degranulate the socket with a molt currette and a surgical length coarse diamond. Does this patient really need a replacement lower second molar with an implant??
Ed Dergosits
10/25/2019
I would extract the tooth and make certain all granulation tissue is removed and the socket cleared of any residual PDL cells. Does this patient really need to hae this tooth replaced with an implant? It can be done but I would proceed only if she asked for the implant.