Radiolucency around coronal portion of the implant: next steps?
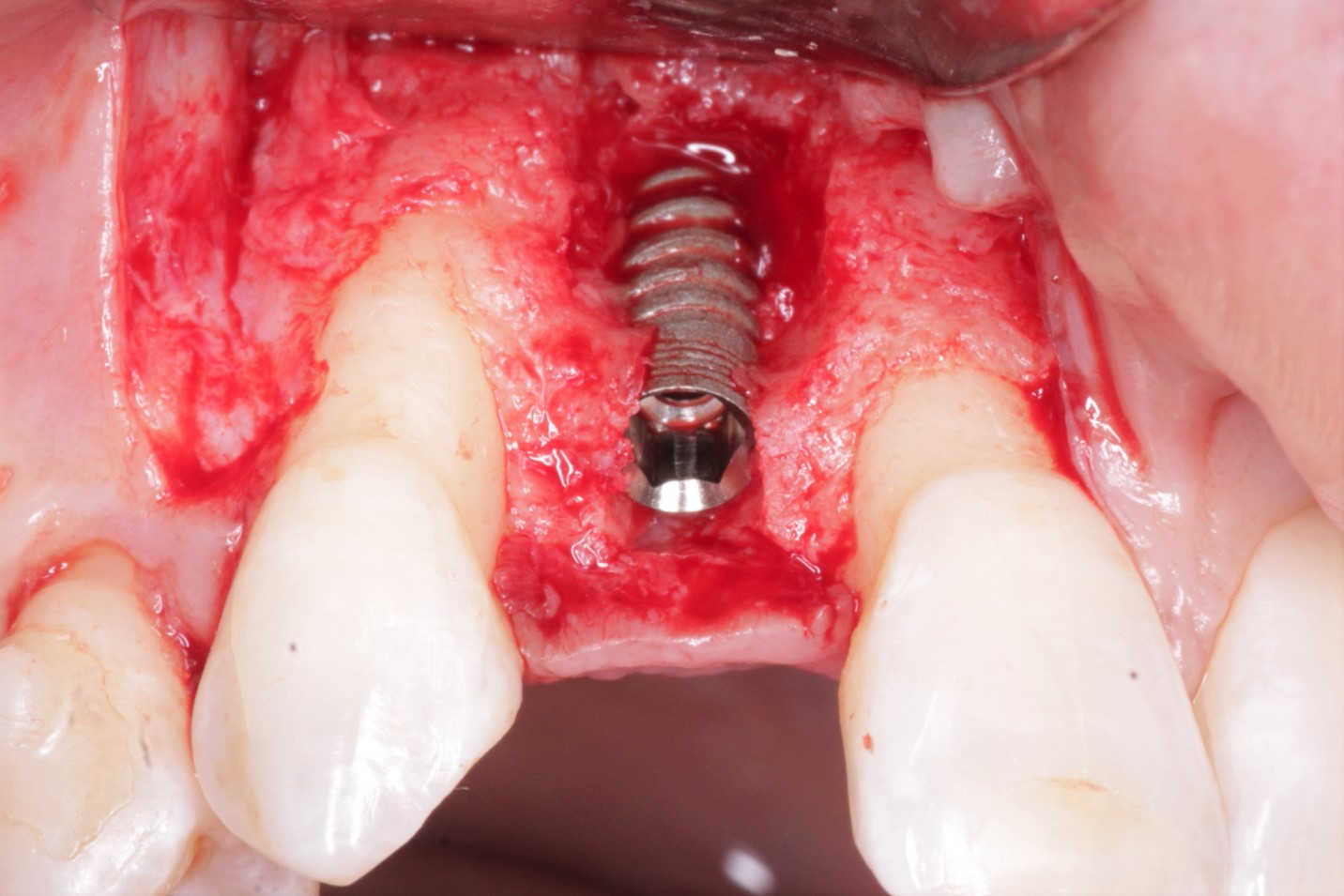
The patient is a 64 year old healthy male patient. The patient had a vertical root fracture with previous endo on tooth #3 [maxillary right first molar; 16]. The tooth was extracted with no complications and grafted with 50/50 cortico/cancelous bone. After 5 months of healing, the implant was placed. Good primary stability was achieved and healing screw was placed. The tissue was sutured and the patient was seen for 2 week post op check. There were no complications at this time. The patient was seen 4 months later for uncovery and the top of the implant was exposed. The radiograph showed radiolucency around coronal portion of the implant. I tried to unscrew the implant but the implant was stable. What is my next step in this case?
![]implant-picture-2](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2014/03/implant-picture-2.jpg)
![]implant-picture](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2014/03/implant-picture.jpg)