Afterthought: Was Immediate implant best tx plan?
First solo case, but not my first implant placement though. I have enjoyed seeing other cases here and I thought I would share my case and get some feedback. I placed a few implants (not enough!) in my Air Force training and career.
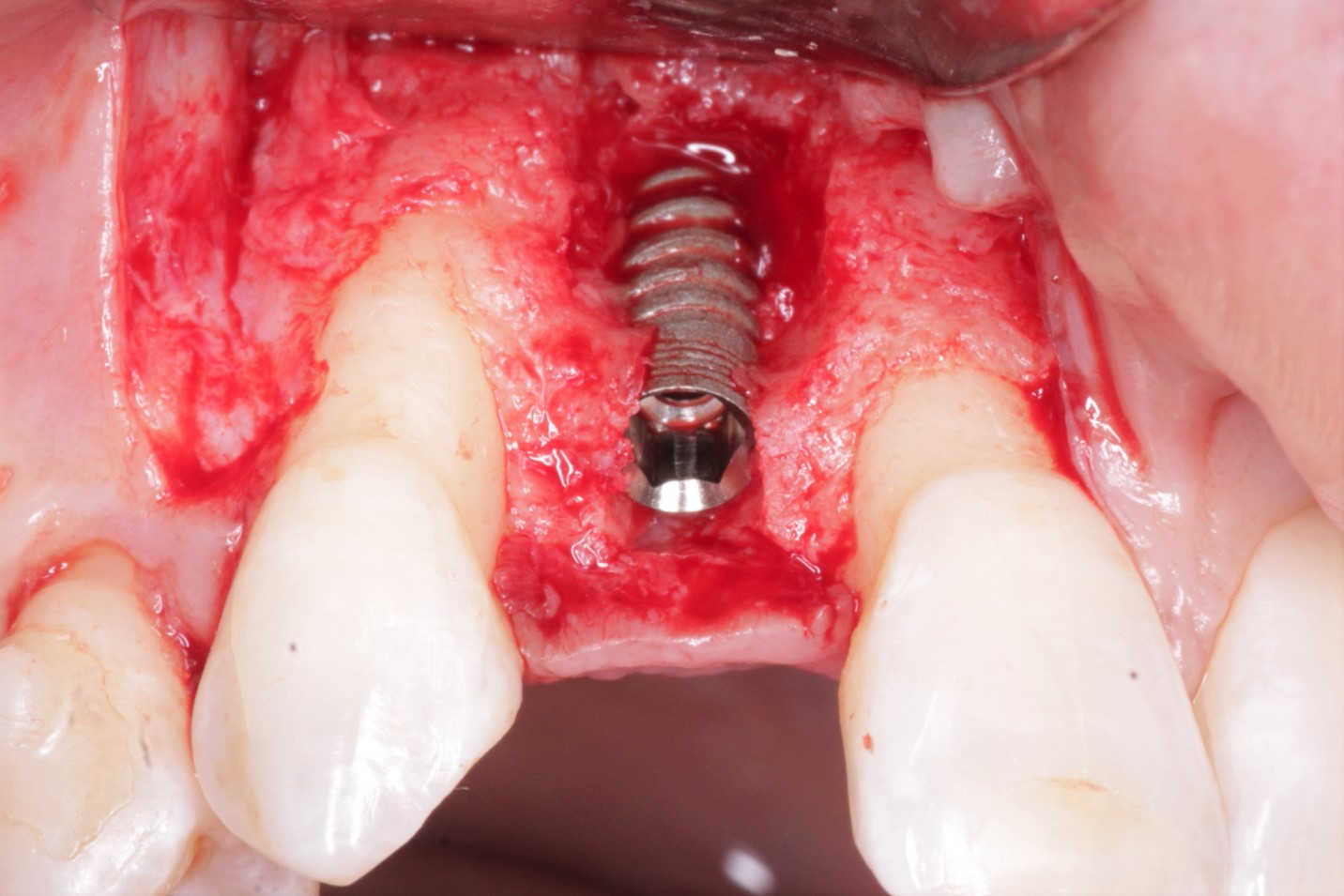
I have a 50 year old male non-smoker with deciduous T [primary tooth]with class 3 mobility. There was 4 + mm of keratinized gingival tissue. The treatment plan was to extract the tooth, place an immediate implant and graft if necessary. Final restoration would be a crown.
I made buccal/lingual sulcular incisions to distal of adjacent teeth and carefully reflected a buccal flap to view the bone structure. I extracted T and de-granulated the area. I placed an OsseoSpeed 4.5 X 11 mm implant (Astra Tech). I may have placed the implant 1 mm more apically than I planned from the CBCT™s. I apologize for the angulations in the periapical radiographs. The buccal plate was thin so I decided to graft with mineralized cancellous/cortical and covered with PTFE membrane. I sutured with 4-0 silk sutures (horizontal mattress, 3 interrupted).
I saw the patient for a 4 “day post-op and he is healing well. No facial swelling, no paresthesia, and little discomfort. I will see him in 2 weeks to remove sutures and deliver a flipper.
Looking back I wonder if grafting the area for bone loss on the mesial of #30 would have been a better tx option? I appreciate your feedback.
![]implant3d-v2](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2013/12/implant3d-v2.jpg)
![]implantguidedrill-v2](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2013/12/implantguidedrill-v2.jpg)
![]implantfinal=v2](https://osseonews.nyc3.cdn.digitaloceanspaces.com/wp-content/uploads/2013/12/implantfinalv2.jpg)