Complex Medical History: Should I Proceed with Implant Treatment?
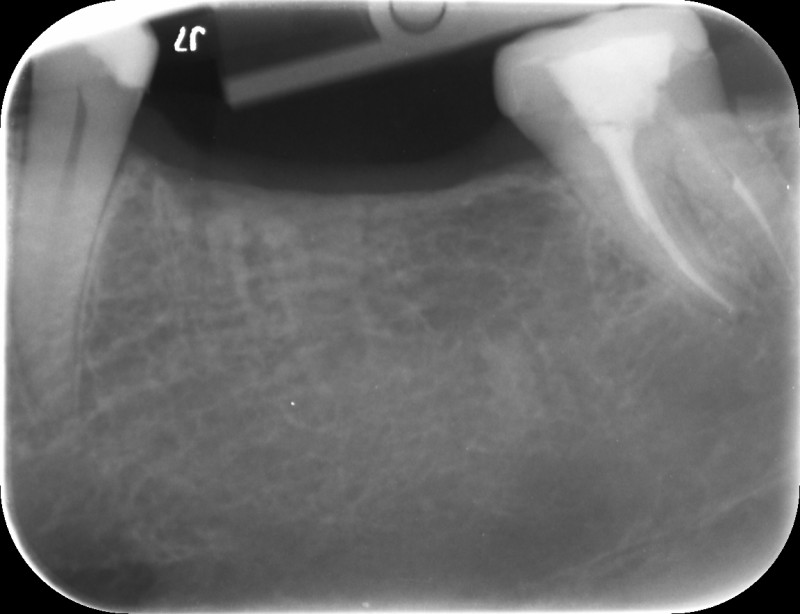
This 39-year old male patient would like implants to replace #18, 19 and 30. Clinically and radiographically there appears to be sufficient bone (see attached x-rays). The problem is that he has a complicated medical history.
He has suffered avascular necrosis of both hips requiring hip replacements. This was caused by pancreatitis, as a result of alcoholism. He is now off alcohol.
His daily medication includes ciraplex 10mg, gabapentin 600 mg, oxycodone 15mg, klonopin 0.5mg-2mg,morphine sulphate 60 mg,omeprazole 40 mg, simvastatin 20 mg, multivitamin and fish oil
It appears like a great case to do surgically but I’m concerned about his medical history.
Any thoughts whether I should provide treatment?



19 Comments on Complex Medical History: Should I Proceed with Implant Treatment?
New comments are currently closed for this post.
Jawdoc
3/20/2016
1. How's the blood cholesterol/lipid profile?
2. How's the blood sugar level?
3. How's the pancreas function (any pancreatic function tests done?)
4. How's the liver function?
5. How's the full blood count?
6. How's the psychological profile of the patient? (Motivated, optimistic/pessimistic, Easy-going, difficult, depressed, anxious, etc?)
7. How's the oral hygiene & dental history? (Any history of complications after extractions &/or surgeries (eg dry socket etc)?
8. Any other med conditions? (Eg bleeding disorders etc?)
If it's an all-clear/ a-ok for all the a/m, then go for it. All the best! Interesting case, thanks for sharing!
CRS
3/20/2016
It seems like this is a chronic pain patient with a significant amount of opioids in his system and a recovering alcoholic with significant systemic damage. One addiction substituted for another. The Big red flag is the bilateral a vascular necrosis of the hips. Patient may very well have advanced vascular issues with poor perfusion and chronic liver, pancreas issues. Remember dental implants are elective, the hip replacements were not. Is this person able to work and function? I would be extremely cautious. Remember that mental health issues are relative contraindications to dental implants. On the other hand if the hips are doing well and integrated and the patient has strong psycho-social support and is not chronically disabled, the dental implants may offer the patient the ability to eat better and feel better. I have treated debilitated patients with success but I make no promises. The patient has to accept that the implant prognosis is guarded and they may fail.
I like to evaluate the patient as a whole and see how well they heal as treatment progresses.
LDRN
3/31/2016
CRS, question from a lay person; why are dental implants contraindicated in clients who suffer with mental illness?
Alex Zavyalov
3/22/2016
It looks like the patient’s adjacent teeth have been perfectly restored, and he does not want to touch them. With his medical history the risk of unpredictable complications is rather high and he won't get a functionally better result from implant placement than from conventionally made bridges. I would refrain from an implant treatment plan here.
Jawdoc
3/22/2016
This is an interesting case that attracts opinions from both ends of the spectrum. One being proceeding with the implants ( & having the obvious benefits they impart as opposed to conventional RPDS/ FPDs) after checking/considering all variables to be in favour of (or at least, not being in diametric opposition to) the placement of implants; & in so doing, assuming some risks of the unknown. The other, of not assuming any risk at all in relation to implants & in so doing, opt for FPD - which is a perfectly feasible alternative ( though ironically, not absolving one from the conundrum of the downside/ disadvantages of conventional FPD). I would say all points of view so far make sense in their own ways. This is part of what makes this case interesting :)
DrT
3/22/2016
Also would like to know if he smokes. I would probably consult with his orthopedic surgeon as well
Dennis Flanagan DDS MSc
3/22/2016
At a minimum this pt is a poor healer. I would advise an all mini implant splinted supported crowns. Narrow occlusal table, 2.5X10mm implants, cemented (obviously) and 4 month recall. The minis have much less osseous displacement and percutaneous exposure than standard implants, thus less of a risk for peri-implantitis if you get integration to begin with. I feel strongly about this from my own experience and publications.
Dennis Flanagan DDS MSc
sergio
3/24/2016
Agreed. Small diameter implants will work very well here as long as occlusion is in check. I noticed with sdi's when multiple get splinted, gingival inflammation occurrs often if pt. slacks off on hygiene. Nevertheless, it works well in this kind of situations.
Dr. Gerald Rudick
3/22/2016
CRS HAS SAID IT "RED FLAG IS UP"
REFER HIM TO SOMEONE YOU DON'T LIKE...THIS GUY IS POTENTIALLY BIG TROUBLE!!!!!
Jack Yetiv, MD. PhD, JD
3/22/2016
I am not a dentist, but I am a physician (ER doc) with a PhD in pharmacology and a law degree. I think the above comments are very good, but I have a couple more to offer:
1) I am concerned about any individual who takes oxycodone AND morphine sulfate on a chronic basis.
2) You say he is "off alcohol" and that may (or may not) be true. Given his motivation to get implants, his self-report of being alcohol-free may not be reliable.Even if reliable, recidivism risk is rather higgh, especially for someone who probably has an opiate addiction in addition to his alcohol addiction.
Based on the limited info you provided, it's probably not appropriate to offer a recommendation for you to proceed or not, but what I would recommend is that you call his primary care doc in addition to his orthopedist and see what they think.
And the lawyer in me says that if you proceed, and as suggested above, you should disclose a high chance of failure and have the patient sign ff on it.
LSDDDS
3/22/2016
Again the heretic but in concert with JawDoc
Observe abutments (and many other teeth) heavily restored and hence ideal for full coverage and here fixed bridgework eliminating the concern of osseo integration. Perhaps start with a single crown elsewhere as trial for I must agree with Dr Rudnick that there could likely be other management Issues given the history.
Sometimes remuneration is not worth aggravation
kent hamilton
3/22/2016
I would not do an bridge, Look at the decay on #2. This patient will continue to have uncontrollable caries. But the dilemma is that implants which in his mouth are the best treatment option are NOT the best healing option
I would first get a medical clearance from ALL of the MDs involved in his continuing treatment.
Dr. Vipul G Shukla
3/22/2016
This case raises MULTIPLE Red Flags as Dr. Rudick has noted. An ex-alcoholic has now transitioned from liver, hip and pancreas-damaging alcoholism to brain-numbing, stupor-inducing narcotics & benzodiazepines. What are these for anyways? Once total hip arthroplasty is done and integrated, there is minimal discomfort or pain to the patient. By the way, chronic pancreatitis and AVascularNecrosis(AVN) of femur heads from chronic alcoholism is well-known. ALL cortical bone in the body is affected to one degree or another, so expect some reduction in vascularization of mandible as well. It is said most effects reverse if you stay dry for five years or more. This gentleman is possibly staying dry now since he knows he only has one liver. The statin is because he does not metabolize fat properly anymore. Ask him if he is on a low-fat diet. Ditto fish oil. Same reason. Omega-3,6,9 is considered to reduce your LDLs.
Pancreas secrete Insulin and Glucagon too. Also Somatotropin. For digestion, pancreas secrete chymotripsin and other digestive juices that help break down all type of food in the early small intestine, especially fatty food.
I'm surprised he is not an insulin-dependent diabetic already. Maybe he quit on time and maybe he has good genes.
Where does he work? Who will pay for these implants? I don't know any dental insurance plan here in Canada or even the US that will cover such comprehensive prosthodontic treatment. Will he put down say, $6000 as a deposit then you evaluate further? See how that conversation goes.
Maybe he is dry now and his liver tests and CBC all come back normal. Perfect sugar metabolism and no AVN of mandible either. Perfect candidate. So why is he on all kinds of narcotics and benzos and Cipralex? And Gabapentin? Does he have diabetic neuropathy? Seizures? Trigeminal Neuralgia or Shingles pain? In the last 2 years, Gabapentin has been investigated as a drug of abuse, especially in a Drug cocktail. It is supposed to make you go into a trance, a weird high when mixed with other narcos. Google it.
I would restore the upper right molar interproximal cavities first and then evaluate this patient carefully.
Very very carefully.
Good Luck!
The other Dr.T
3/23/2016
I would NOT recommend a bridge until he is free of decay and able to maintain it. With his visible dental history, he is obviously high risk of failure due to recurrent caries. Do you really think he'll thread floss under a bridge to keep it clean or he going to let it decay away? I know you guys like the money a bridge gets you, but what's best for the patient? Make a removable partial so he can take it out and clean his teeth. If he can go a few years without new decay, then do the fixed bridge. If you do FPDs now it's a disservice to him. You're just stealing his money. Would you put braces on a kid with decay? No. You make them prove they can keep things clean first (or you should be).
Patients have to earn fixed bridges.
vijaykumar bokkasam
3/23/2016
Avascular necrosis in this case could be due to fat embolism of end arteries which is unlikely to be seen in jaw bones but at the end of long bones.As the patient is in good health now , away from alcohol, I think he is like any other patient to investigate except for additional LFT and go for implant.
Roxanne
3/26/2016
As a patient who has a complex medical history (salivary duct adenocarcinoma, parotidectomy, 66 grays of radiation with late onset of Osteoradionecrosis of the left mandible resulting in an osteocutaneous flap to replace the mandible and on gabapentin, tramadol and hydrocodone with acetaminophen) and anticipating to have an upper right implant next week, I found this to be an interesting conversation.
I am not adequately educated in dentistry to make a statement regarding the implant. Although, I'm not a doctor nor ANY medical professional, I'm sufficiently knowledgeable about my personal circumstances with the drugs to say that they don't necessarily lead to trances or highs. Admittedly I'm not familiar with all of the drugs that the patient is taking; nor have I been an alcoholic.
In terms of addiction, this is something of sufficient concern to me that I saw a neurologist (not involved in my pain management) to learn about alternatives to the meds. He talked to me about trigeminal ablation, but suggested that given my age (58) and the risks of ablation he would encourage me to stay on the drugs and suggested that I could ask to have the gabapentin increased as the jaw pain is still chronically present although minimized.
CRS
3/28/2016
Different scenario and etiology. Hope you have received HBO as a precursor to treatment of any bone in the line of radiation if indicated prior to implant placement. I have a similar case and we will place maxillary implants once the patient is stable from his adenocystic carcinoma. Good health to you and thanks for posting. Great patient viewpoint.
Roxanne
3/30/2016
Thanks CRS.
The implant will be on the non-radiated side. No HBO.
I did have it prior to earlier surgeries intended to arrest the ORN, but in hindsight the HBO may have been too late to help much.
broach1
4/5/2016
great discussion, thank you
but lets not put the " implant cart before the horse"...
lets do caries elimination, endo on 4 and 14 and probably others; and assess those third molars and his plaque control over the next 6 months than revisit his medical progress or recidivisim.He will live just fine with those spaces for now .














