Gingival Recession Case: Is There Any Solution?
Dr. H. asks:
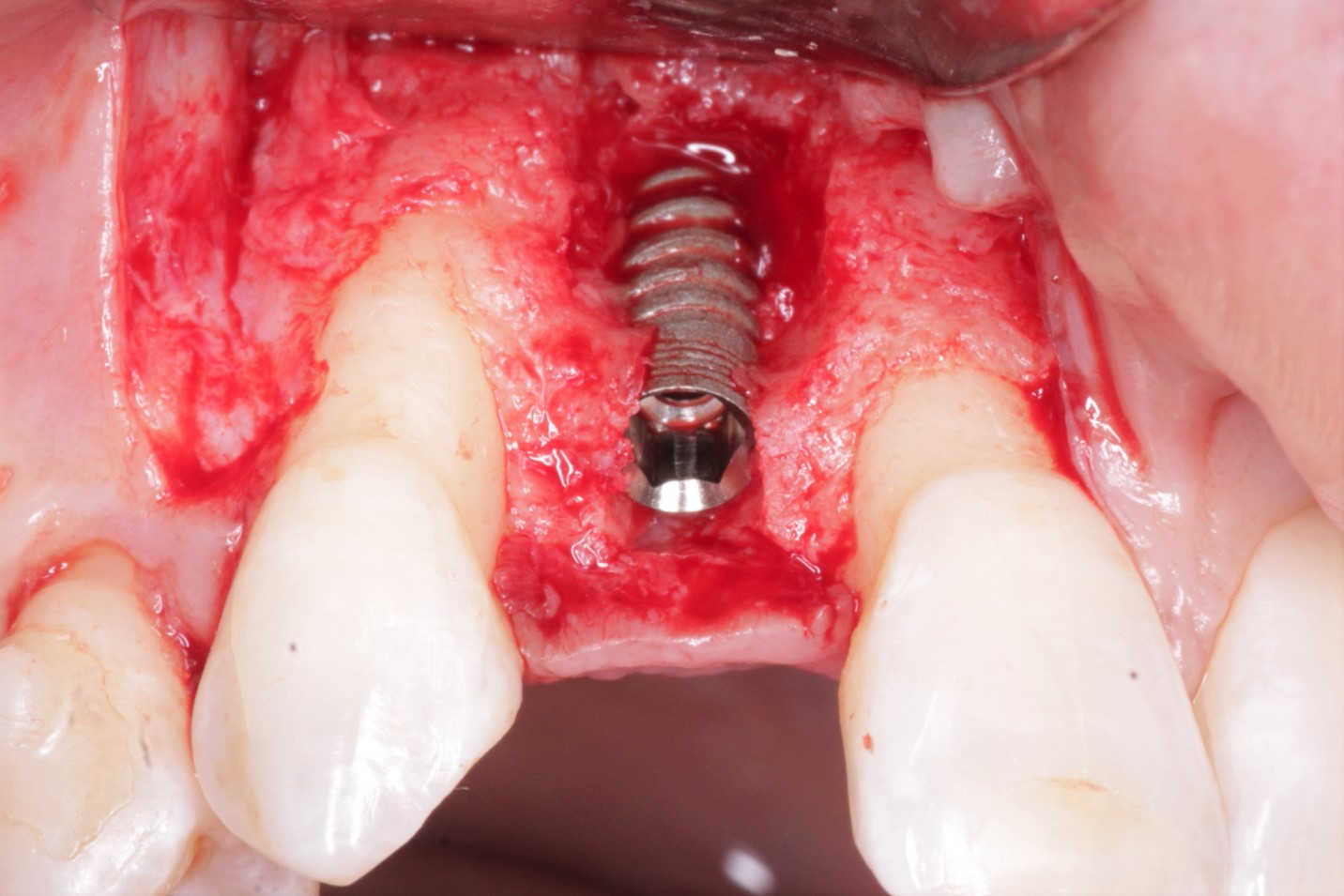
Please the case photo below. I have a complication now that I am not sure how to treat. I placed a Biomet 3i implant fixture in #9 site [maxillary left central incisor, 21]. After 7 months, the implant fixture appeared osseointegrated and there were no signs of inflammation or infection. I uncovered the implant platform and healing cap and placed a transmucosal healing abutment. The patient returned in 1 week for final impressions and presented with inflamed, swollen and receded gingiva. This is a critical area for aesthetics and I need to find some way to correct this complication. What do you recommend to do about this horrible gingival recession? Is there any solution?

23 Comments on Gingival Recession Case: Is There Any Solution?
New comments are currently closed for this post.
Dr. Morales Schwarz
1/17/2011
The best treatment is to start again from scratch.
Remve the implant, place a provisional restoration, graft with an autologous bone block either from the palatal area or from the chin, wait about three or four month, place a new implant in an ideal 3D position, free gingival graft, impression and new crown.
Its a challeging case.
Good luck.
Shirley A . Colby
1/17/2011
The picture presented is blurred in some areas. Gingival margins on other teeth not well defined. Looks like they're manifesting some form of inflammatory gingival irritation, from the braces perhaps? This could have precipitated the infection of the implant.
How young is the patient? How meticulous is he about oral hygiene? Are there any possible systemic conditions that may contribute to this situation?
From the looks of it, an infective agent is involved in the equation, but check for pre-maturities, nevertheless.One needs to ascertain the root cause of this condition before starting over. Otherwise, one may end-up repeating the same process.
Jack Wu
1/18/2011
Can you please show the photo before you place the abutment and the xray of this case? From my point of view, the recession may cause by the op you do for the abutment placing or there may be a trauma biting on the provisional crown.What Dr. Morales Schwarz had suggested may be the only way.
Good luck
mike ainsworth
1/18/2011
looks like anug to me.
Is the patinet a smoker? immonocomprimised in any way?
Treat as an aggressive ANUG. LA-take off the cap, fully clean, leave cxd gel on and inside the implant for a few mins, rinse with sterile saline. full mouth scaling. dry, fill the implant with chloramphenicol eye drops, place a sterile submerged healing cap on the implant and prescribe Metronidizole and Amox in combination for 7 days + multivitamins and Iron. Cxd mw 2x 1min per day
wait and see... you amy need to do more but no way of knowing until the acute phase is over.
Hope this helps
dr.p
1/18/2011
1-remove provisional
2-place cover screw.
3-sent pt home with peridex for 14 days
4-place connective tissue graft (or allograft) burying the implant.
5-perform frenectomy at the same time of graft
6-uncover implant in 12 weeks
and then start molding the peri implant soft tissues.
(start with a very small emergence profile healing abutment or provisional and gradually increase the emergence profile)
and good luck and thanks for sharing
mike ainsworth
1/19/2011
I agree a graft may be necessary, just make sure you have full tissue maturation post infection prior to doing this. If you are not 100% comfortable with this technique send it off to a perio that you trust, this is not a case to start on-too many variables.
good luck
peter fairbairn
1/19/2011
Hi Spanish boys David and Mike , agreed here nightmare case an x-ray would show more as the implant is placed too deep and looking at the angles possibly too close to the lateral . But a difficult case might need to remove as graft unpredictable.
Peter
Dr. Samir Nayyar
1/19/2011
Do send the patient to a periodontist.
abdusalam alrmali
1/19/2011
treat the gingival inflammation first,motivate the pt to perform a good oral hygiene, take a radiograph to determine the level of bone support around the implant and the tooth adjacent, measure the amount of keratinized gingive around.
i donot advaice you to remove the implant because its proper osseointegrated as you said, so we have to prevent spread of the inflammation more deep.
think about the cause of this mistake to complete the circle.
thank you
jg
1/19/2011
An x ray, would help....Did you by any chance left recidual temp. cement subgingivally..? It could produce this type of reaction....
mike ainsworth
1/19/2011
evening peter london good I hope!
Just another point as an aside-dont let the orthodontist take the brackets off for any reason, i think you are going to need them later to finesse the gingival levels. Try to persuade the patient to but braces back on 3-4 months after they come off and see what reaction you get! better just leaving them on if only just in case.
Dr. Morales Schwarz
1/19/2011
Hi peter nice to know we are in the same wavelength,
Looking deeper into this case I have a few more observations.
As you can appreciate the gingival margin of the lateral incisor (Nº 22 or 10) next to the implant is also deeply receded, even to the level of the implant supported crown we are all talking about. That means that Nº 22 has a facial bone dehiscence, caused either by the implant surgery (as Dr. Faibarn pointed out the implant seems to be too close to the teeth) or as a consequence of inadequate orthodontic movement (the teeth is severely tilted to the buccal). Since treating those kind of recessions around teeth is even harder than around implants the following could be a possible treatment plan in case your patient doesn’t want to go ahead with grafts and all that stuff.
First clean everything.
Place a free gingival graft, to avoid further bone loss around the implant and the lateral.
When everything is stabilized, redo the crown and apologize to your patient.
Dr. Shiraki, mex. DF.
1/19/2011
A orthodontic treatment at the same time of an implant treatment, its a very carefull case, the oral hygeine care its a the principal goal.
Remember the soft tissue depends to bone level, if you have a pour bone level in the lateral and the other central teeth, your soft tissue level its pour and the heigth of the prosthetic abutments need to be more longer, Im agree to Dr. morales.
Start again, good luck and thanks to share this.
Dr. Seyed Jalil Sadr, Pro
1/20/2011
For any case presentationand giving comments,we should have more information . Just one slide could not provide all data.
Please :
1- show the Radiograph before orthodontic begin
2- What was the cause / etiology of lost #9
3 -the # 10 also have problem of reccession
4 -the gingival Biotype is (was) thin and scollaped which is of one reccession causes after implantation especially with less than 1mm bone thickness in buccal surface.
5 - I think it is worthed befoe Xplant to open area for cleaning and bone grfting and membrane to regenerate bone and tissues to cover the reccession area.
6 - By the why How is patien lip line from esthetics point of view? if is low, some how is easier to handle, but if is high lip line then a very big complication and even failure.
7 - if esthetic demand is high, the gingival level on # 6, 7, 8, 9 , 10 , 11 make it solutions more dificult.
Finally : to start any case we have to put enough time to evaluate all the aspect and have consultation with other dentist and speciality or Ask help for treatment Planning in this site before touching patient and post the case at least with 8 intraoral picture and radiograph with Medical and dental histories.
Sorry for my useless comment for this special case. I hope it could help for futur cases.
Respectfully about others comment
Dr. Sadr Tehran, Iran
Dr. Jim Dickson
1/20/2011
I am a periodontist and this is a challenging case for anyone. It appears that there is instability of the anterior gingiva. Someone is going to have to surgically open the area to determine what is happening with all of the anterior teeth. I would place Arestin and allow at least a week before opening. It may be that bone grafting and membrane(s) are necessary. It may be that soft tissue grafting is necessary (on more than one tooth and possibly in addition to the bone grafting). It may be that the implant needs to come out and the resulting ridge defect repaired so that another attempt at placing an implant would be successful. This will probably require multiple procedures no matter what is found upon flapping the tissue. I don't agree with apologizing to the patient. In some cases, we run into complications beyond our control. Sympathize with the patient sincerely. This case is a case for experienced hands only!
THoang
1/23/2011
Hi,
Look like the patient is affected with periodontitis. there is loss of interproximal bone between #8 and #9 and btw #9 and #19. Gingiva is inflammed in general. In this case, both implant and ortho need to be delayed until active periodontitis is arrested and controlled.
You may need to send patient to a periodontist for comprehensive periodontal evaluation. if there is lack of vertical height due to bone loss, bone graft is unpredictable for implant but may possible for #10 if an infrabony defects were present. You may try a thick connective tissue graft that would bury the implant, then uncover and provisionalize. Another approach is to bury the implant and fabricate a traditional three unit bridge, this will have more chance to fix the ugly recession and uneven gingival margin. Anyhow a full mouth radiograph would be very helpful.
THoang
1/23/2011
Sorry, i made a typing mistake, #10 not #19!
mwr dds
1/25/2011
Very sorry to say that the implant looks like it's placed too buccal, too deep and too close to the latertal at an angle. I had one like this and apologised to the patient. I removed the implant, and grafted the site and then waited 4 months. Started all over and all is well. Again, sorry to be in this position. Your case looks like a frenectomy is also needed. regards, mwr
jawahir aljahmi
1/26/2011
biocompatiable material it is not harmfull and the implant one of theem so ther is maybe other cause for recession maybe the bracelat
dr varundahiya
2/2/2011
ideal way is to go witj dr.P but practically due to periodontitis in upper anteriors a prior treatment of gum infection was necessary before implant placement.lack of attached gingiva is main factor here which should have been taken care before implant placement.if nothing else work..cervical pink restoration on this crown only can mask the problem if implant is stable.chances of implant loss will persist if periodontitis is not treated.systemic check of sugar level (diabetes) must and repeted recalls to check progress of bone loss are needed.Hope for best.thanks for sharing.
Gary D. Kitzis DMD DABPer
2/6/2011
At the risk of sounding as if i have a conflict of interest, I would sent the patient to a periodontist. There are a few reasons that the area could have appeared good until the implant was uncovered. The one most likely (without seeing any stage two/uncovering radiographs) is that the healing abutment may be too wide, not be fully seated or got loose which caused the inflammation at the level of the fixture/abutment interface or the implant may be too far to the facial, causing recession.
I would replace the cover screw and do a connective tissue graft to regain the gingiva. It is probably not necessary to remove and replace the implant which would require a bone graft, significant time in healing and a considerable increase in treatment time .
Dr. Karoly
2/7/2011
You clearly have very little understanding of implantology. You should NOT have treated this patient.
There are at least three major mistakes that I can see.
Send this patient to a periodontist NOW.
Rui Martins
2/16/2011
In summary, without x-ray there is a lot of speculation about implant position in general. I would't go as far as saying you need to send the patient... or stop placing implants (how else do we learn except with complicated situations?) you will obviously have to remove the crown and follow concensus about treating soft tissue and check about repositioning implant, bone grafting etc. I am curious about implant osseointegration due to orthodontic movements. I sugest fixing the crown, or making a new temp crown, to the ortho appliance and not to implant till after ortho treatment and soft tissue recuperation.
hope I helped