Lower anterior implants: Cause of Unexplained Pain?
I have a 40 year old male patient. Three weeks ago, I removed an implant from the 3rd quadrant in the canine area and on the same day placed a NobelActive implant in each of his mandibular lateral incisor sites. I achieved a primary stability of over 45Ncm. I placed cover screws and closed both implants with a flap leaving nothing exposed. Three weeks later the patient still has 4 out of 10 level pain on the pain scale which was reduced from an 8 out of 10 on the day of surgery. The patient still has to take analgesics. There was no evidence of infection, exudate or purulence. What could be the cause of this continued pain?
41 Comments on Lower anterior implants: Cause of Unexplained Pain?
New comments are currently closed for this post.
Doc
3/16/2018
Not sure the reason, but would you consider a CBCT to evaluate positioning?
George Hetson
3/16/2018
If you don't have a cone beam you have no way of knowing if or what the problem is. I have been doing implants for 35 years ,so I have done many without a cone beam ,since we didn't have them 20 years ago. Now I refuse to do an implant without a cone beam.
Adrian
3/16/2018
A possibility is that the anterior loop of the inferior dental nerve (exiting at the mental foramen) may have be compressed by the placement of the implant, more so with a Nobel Active which displaces the bony walls of the osteotomy. Your patient is probably experiencing dysesthesia which is an altered sensation as a result of nerve damage. Like the others here, I would recommend a CBCT of the area, specifically to see if the implant has impinged on the anterior loop of the IDN. Treatment modalities include - explantation, treatment with high dose steroids, in serious cases nerve resection, ref to neurosurgeon, etc.
A
3/16/2018
Hi.i never give a block when i place an implant so that the nerve is alive while im drilling.so its not possible that im close to the nerve
A
3/16/2018
Hi.As i said i dont give a block while placing implants in the lower.I just give infiltration.So being close to the nerve is not possible otherwise patient would have jumped when i was drilling.
DrDave
3/16/2018
There is not enough medical history. For instance, given the opioid epidemic that we have in US, he you considered that he just might be trying to obtain a few more pain meds. I am left to assume that you’ve had no red flags since it’s ommitted in your “why is he still in pain “ query. Not being facetious
Raul R Mena
3/16/2018
Impossible to advice without XR
Dok
3/16/2018
Three weeks post op is just not enough time to be considering damaged tissues. CBCT in 4 weeks if symptoms persist. Post op pain three weeks out is not that unusual ( I know because my own mouth/implants hurt for that long ).
A
3/16/2018
Ok.point noted
Matthew Osepchook
3/16/2018
I agree with Adrian. I have used CBCT to identify patients who have an anterior loop of the mental nerve which is likely accompanied by a vascular bundle as well. In some cases the neuromuscular canal is apparent all the way to the midline making implants a very difficult scenario if not a contraindication. A post op CBCT is highly warranted here and I would love to see if the implant has violated some anatomy that otherwise is usually not an issue.
A
3/16/2018
Hi.As i said i dont give a block while placing implants in the lower.I just give infiltration.So being close to the nerve is not possible otherwise patient would have jumped when i was drilling
FES, DMD
3/16/2018
One of the comments mentioned refer to a Neurosurgeon. Why in the world would you do that??? Oral and Maxillofacial Surgery is the specialty that is best trained in the management of nerve injuries involving the maxillofacial region, not neurosurgery. Referring this to a neurosurgeon would not be in the patient's best interest at all and most likely result in the neurosurgeon laughing at you, for not phaving a better understanding of their expertise. If you dont feel comfortable managing this, find a well trained OMS and discuss the case with him. Not to be condescending, but if you cant manage the complications, maybe you should reconsider performing the procedure.
Richard Guerra
3/16/2018
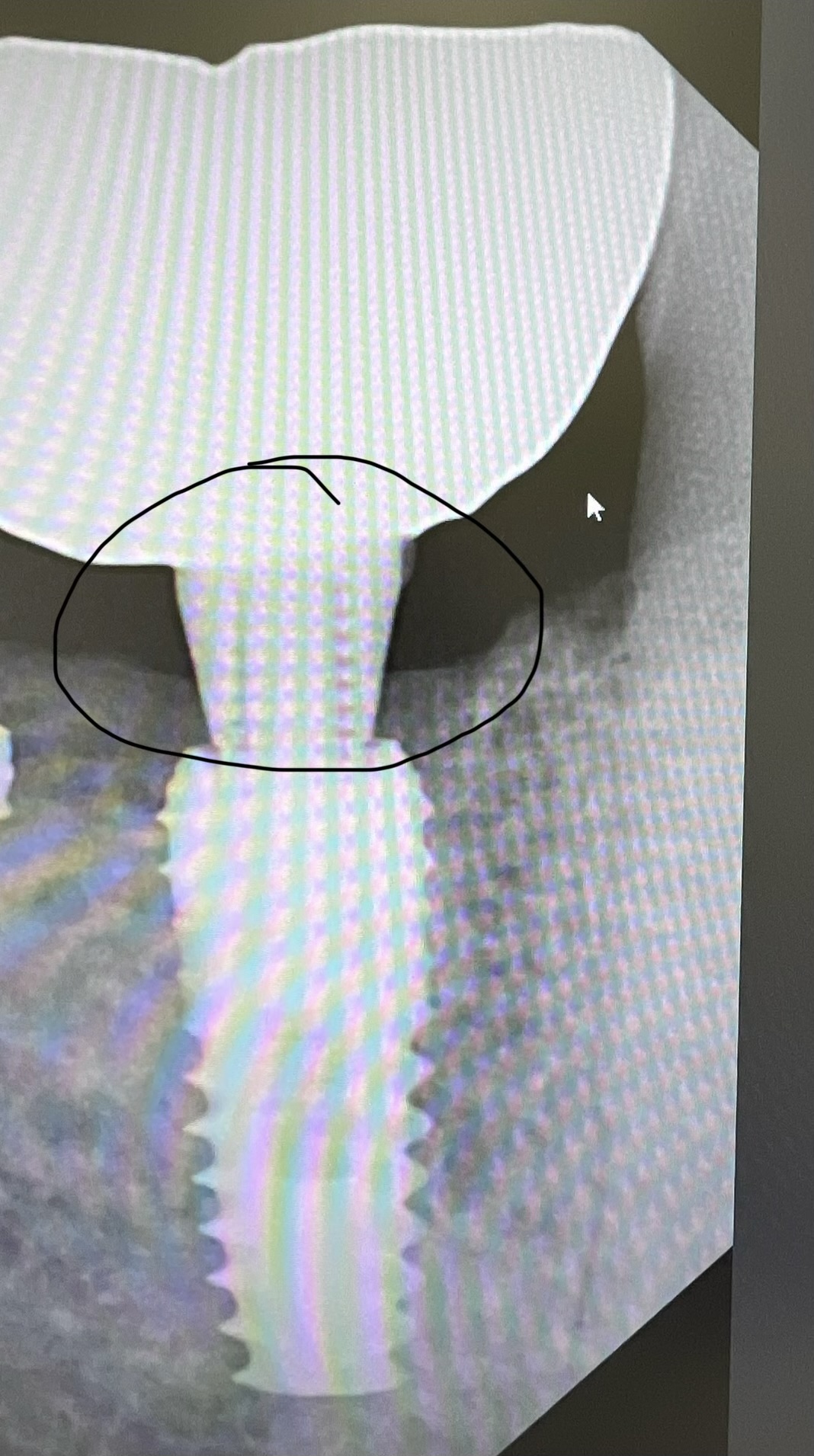
Sounds like a few cbct salesmen on here. With the acceptance and trend of using shorter implants CBCT should be less necessary than in the past. Provide more info. What are the dimensions of the implants? How deep was the osteotomy? How subcrestal was the implant placement? Nobel implants have been known to fracture particularly 3.5mm and below so consider a fractured implant as a possibility.
A
3/16/2018
Both implants were 3mm x 13mm and placed slightly subcrestal.This is a possibility.Can it be a pressure necrosis?or bone necrosis?what if it is?
PA
3/17/2018
fracture of cortical plate?? if not nerve compresstion or necrosis
A
3/17/2018
I think its necrosis.suggestions pls
A
3/17/2018
But wont there be wound dehiscence if there is necrosis?
Dr Anuj Chhabra
3/17/2018
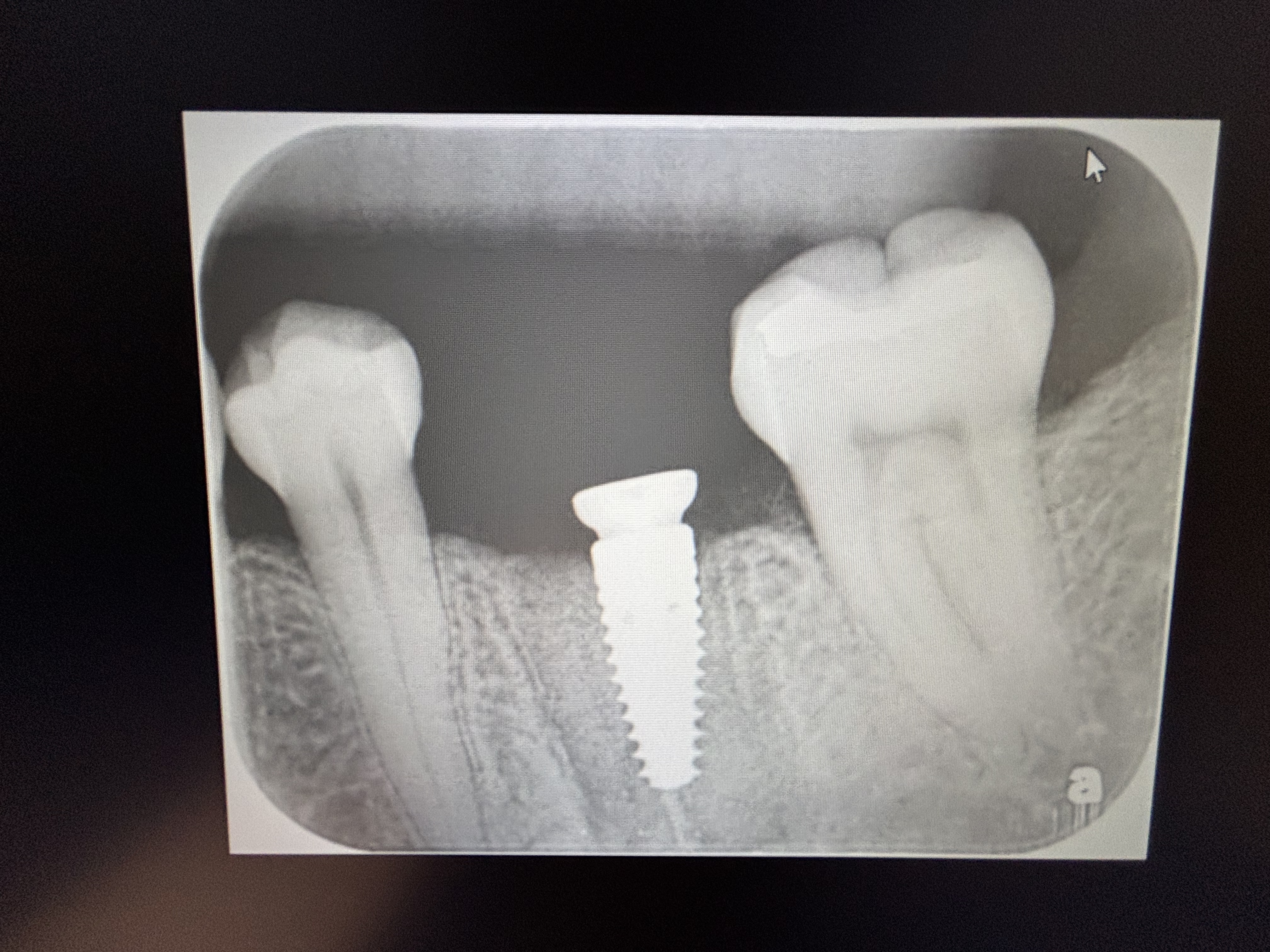
Kindly upload the x-ray images for better understanding.
viet
3/17/2018
How about Myofascial Pain with Trigger points located in
1/ The Anterior Digastric muscle.
2/ The Superficial Masseter muscle.
3/ The Internal Pterygoid muscle.
The Myofascial Pain may exists before implant placement due to parafunctional activities i.e. Bruxing/Clenhing or forced opening of the mandible during surgery.
Please do muscles palpation to make this diagnosis.
Adibo
3/17/2018
It’s funny thinking CBCT is the solution for any biological complications!
The guy seems knowing what he is doing and the symptoms described are not by no means of neurological nature to blame misplacing or implant related neuromyalgia.
I have seen only one or two case reports for neurological symptoms following implant treatments.
Not an unusual scenario with implants, which are ment to compress the osteotomy site to maximise initial stability. Compression necrosis is perhaps the most likely cause and removal of the implants is the only option.
I have had 2 similar cases that I had remove the implants. Sooner you do, easier will be the replacement.
You mentioned that you removed an implant and placed “implantsâ€. Knowing the reason why the original implant had to be removed, may also be related to the symptoms with the the implants ‘immediately’.
A
3/17/2018
Well dr adibo.i too feel the same way-pressure necrosis.but wont the wound dehiscence be a prominent sign?which isnt there in this case.Would u see necrosis on an xray?i think u would though im not sure.whats your take on that
Adibo
3/17/2018
Dear A,
You have a patient with pain! You don’t need to have necessarily adverse soft tissue healing in the initial phase of a compression necrosis. There will also be no radiographic sign of osteonecosis for several weeks until you get the outbreak of the full blown infection. By experience, implants with prolonged post operative pain are failing implants.
B John dds
3/17/2018
Nobel active is a very aggressively threaded implant fixture. You mentioned the 3x13 implant was placed to 45N centimeters. Do you feel that your osteotomy was done the full 13 mm? With underpreparation perhaps compression trauma to the bone occurred in this manor as you suggested. I would consider removing the 13 and placing a 10 if this seems to you that this may have happened.
A
3/17/2018
Hi.yes i agree its possible.but if i put a 10 now i wont get stability.My question now is how can i dete t compression necrosis ?what are the clinical signs?wont there be wound dehiscence?Will the pain 3/10 on pain scale go away with time?
A
3/17/2018
What i mean is if i leave the implant in(as im not sure about the diagnosis of pressure necrosis as yet) will the pain reduce over time?
Kevin Caruana
3/17/2018
I agree that you need cbct as you might have :
1. Perforated the bone plates
2. Entered a nerve canal (breach of the incisive canal is usually found in cases where there is residual pain in anterior mandibular implant cases). It does not happen every time the incisive canal is breached however. I had looked into this and there is some research, but you won't find many articles.
Having said that, why not reverse torque slightly and try retorquing to 35Ncm to see if it helps ?
For those who don't use cbct in lower mandibles and try to defend themselves - please stop arguing against it. If you even remotely care about your patient you would take a cbct to check where you are going.
A
3/17/2018
Thanks for ur comment.i have a preop cbct.nerve is not there.i dont have a post op but im pretty sure i have not vilated cortical plates.i can try detorquing
Adibo
3/17/2018
Dear Kevin,
Nobody is against the technology.
CBCT is a valuable diagnostic tools not a magic wand.
It’s a basic surgical complication and the answer is not to take another CBCT to diagnose it.
Although completely irrelevant for this case, perforation of cortical bone happens from time to time for anyone places enough implants. Do we get the patients back with pain? Where is the physiology of pain in relation to cortical bone perforation?
With regards to the mentioned incisive canal entrance, the surgery was according to the Dr A. in the 3rd quadrant. How big is incisive canal in this area, where the teeth had been long extracted (“the implants were replacing other implantsâ€)?
Please share with us if you have seen even a case report for post implant surgery pain due to implant entrance to mandibular incisive canal?
A
3/17/2018
Ill again reclarify.1 implant was placed in 3rd quadrant lateral incisor area.From same quadrant canine area i removed 1 old implant .in the 4th quadrant lateral i placed 1 more implant.no teeth between these 2 implants.4 unit bridge planned
A
3/17/2018
In the cbct there is no nerve in this area.Im planning to detorque the implants.Problem is i dont know if i should detorque both implants as patient cant pin point the pain
Steve Hurst
3/17/2018
You may want to check with Nobel regarding a 3.0 Active as a bridge abutment. I believe they're indicated for single units only.
Raul R Mena
3/17/2018
Dear Colleagues,
I can see that there are many have given sound opinions as to why there is the presence of pain, but why not start with the KISS Rule.
First of all if you want to receive a valid opinion please send X RAYS.
Start with simple PA and Panorex, and if there is no enough info for diagnosis then go to a CBCT, no need to over radiate the patient .
For many reasons don't delay taking Radiographs and CBCT if necessary, the most important is that if the implant is traumatizing the inerve the sooner you take care of the situation the greater the chances of proper healing and no permanent condition .
Second reason is , legally the patient may decide to go for a 2d opinion ( we all know how prone to criticize is our profession) . If for some reason there is permanent damage and you have not acted within the standard of care now you have no way to defend yourself legally, morally and in front of the Friendly State Board of Dentistry .
A
3/17/2018
Yes i agree dr mena.but i have a preop cbct.there is no nerve in this area in this patient.When i saw this case i thought it is pressure necrosis but i had never seen a case before myself even after many years of implant practice.Once i drilled i did see less blood supply in the area though.Im plannig to get a post op cbct tomorrow
Paul
3/17/2018
Analgesics deal with pain but there could be an underlying cause like low-grade infection that may not be manifested by swelling, purulent discharge or radiographic evidence. Sometimes a short duration of treatment with an antibiotic including metronidazole may be in itself diagnostic and treat the problem. A blood panel may not be a solution either.
Raul R Mena
3/17/2018
D1 bone in the mandibular area in my opinion is the worst type of bone for implant placement.
OK OK I know 90% of you will disagree, but that is my opinion.
When doing an osteotomy in that type of bone and with no bleeding or minimal bleeding use a #2 high speed burr and do RAP , then if enough blood is obtained in the area place the implant.
It is safer to wait 4 weeks and do a reentry.
What type of implant did you place and hopefully you didn't use more than 35 Newtons
Best
Raul
roadkingdoc
3/17/2018
I am alway intrigued by the advice on a forum site. no cone bean needed? ha! I have done many implants in my career. If there is adequate bone, size of implant, depth of implant which avoids the no no areas has little to do with discomfort in my experience.. subcrestal placement is important for restoration reasons but probably not a cause of discomfort. I think implants that hurt are probably infected or have been placed in a weenie dental patient. some of my worst failures never had a complaint from the patient. i like medal dose pac for post op med. I would explain to the patient I see no reason for discomfort. you may have something unusual going on although rare. stay the course or I will remove the implants if staying the course is to tough for you.
Dr G
3/18/2018
Over 10,000 implants placed. I can guarantee you pain after 10 days is a failing implant.
Give it another week if it still is a 4 out of 10 take it out, let it heal for 12 weeks and try again.
Raul R Mena
3/19/2018
Dr. G
Amen
Bill Woods
3/25/2018
Take it out. No reason for any pain over a day which should be from tissue manipulation only.
Cone beam is good to diagnose what is AND what isn’t a possibility but I would wait for healing and go back. Detorqing should have been done first in my view. No long term narcotics ever needed. You can play with biology a little but you can’t fool it. Just remove it. Comfort the patient tat thugs will clear up ad all they’ve lost is a little time. Be humble. Up front. This is the practice of dentistry. . Jm2c. Bil
Bill Woods
3/26/2018
Sorry for the spelling. “That this will clear up†not “ that thugsâ€.... wasn’t using glasses!!
Dr.Malcolm Miller
3/26/2018
There have been cases , presented that describe compression of bone between tight contacts between lower incisors and or implants/ incisors. Not seen this posteriorly as we have wider interproximal bone. I have rarely used botox in a discrete area diagnostically and even once or twice 10% formalin as described years ago by Goldman and Cohen after descerning there is a discrete nerve fiber or bundle behaving abherently. Very rare , but the orthopedic literaure has shown this can happen as well as dental situations like the "phantom " tooth. Nerves are sometimes hard to deal with.