Cytoplast PTFE Membrane Exposed after Augmentation of Mandibular Alveolar Ridge: What Should I Do?
Dr. M asks:
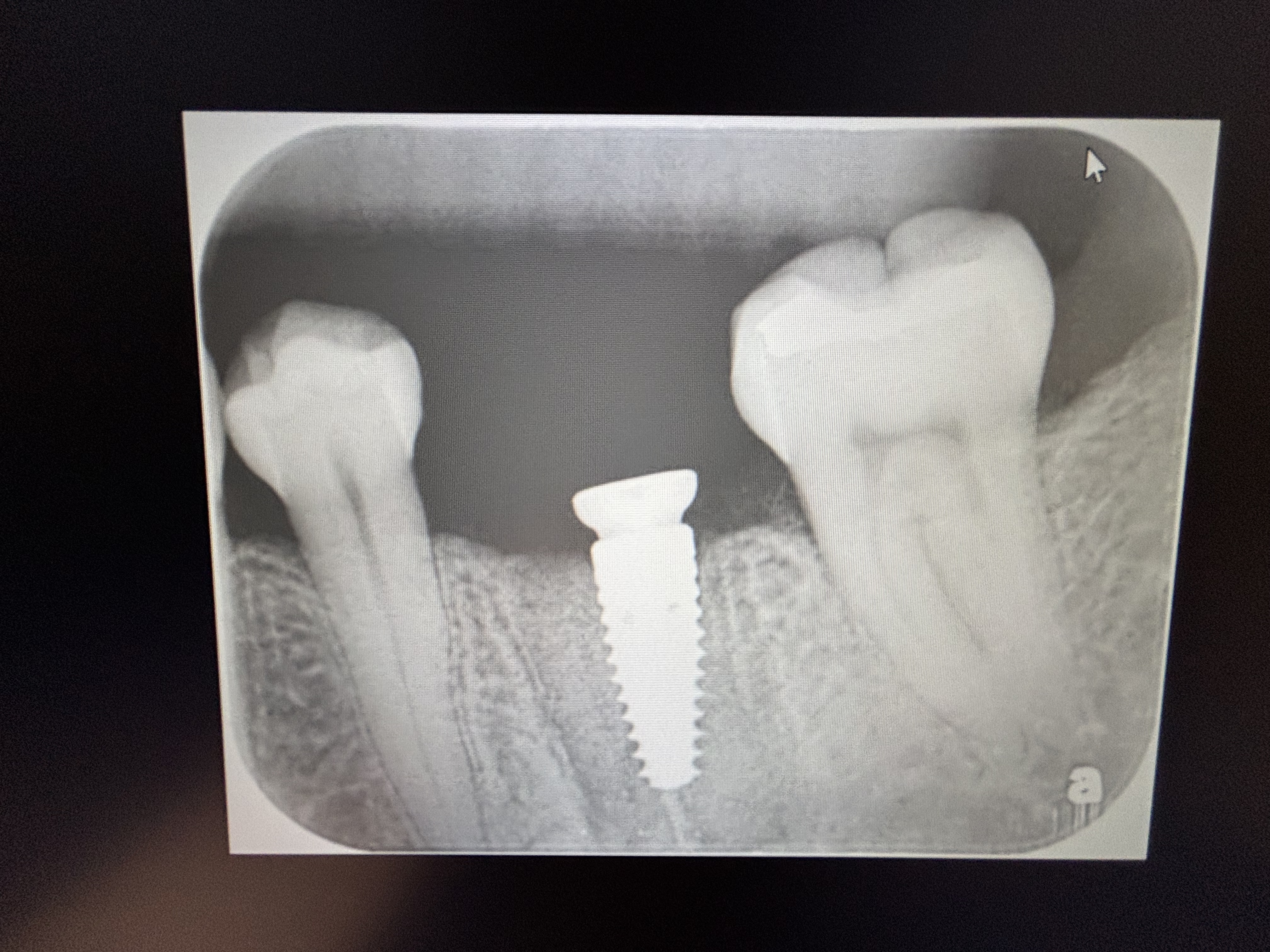
I have a 30-year old female patient with no medical complications that presented with missing #26-24 [mandibular right lateral and central incisors and mandibular left central and lateral incisors; 42,41,31,32].
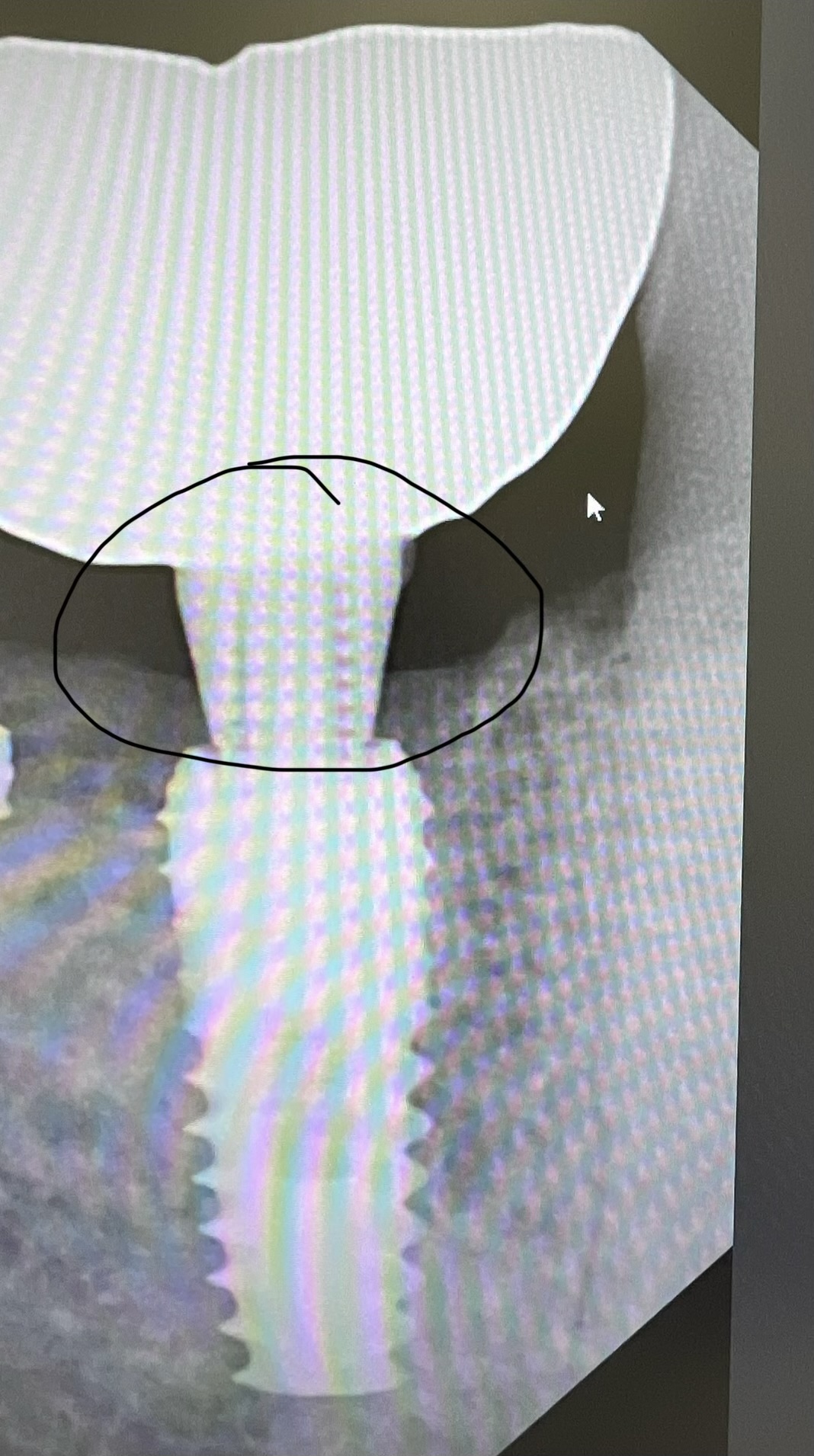
The patient had been treatment planned for a bone graft to augment the thin and short mandibular alveolar ridge followed by a healing phase and then installation of implants. I used an autogenous bone mixed with freeze dried bone allograft and covered with a Cytoplast non-resorbable high density PTFE membrane. The patient returned at 3 weeks post-operative and presented with the membrane exposed. What do you recommend I do at this point?

86 Comments on Cytoplast PTFE Membrane Exposed after Augmentation of Mandibular Alveolar Ridge: What Should I Do?
New comments are currently closed for this post.
Dr.B
10/30/2011
The exposure is too large in this case, you risk infection of your graft. I'd recommend removing the membrane and allowing the tissue to granulate over your graft. If it were smaller, I'd treat with chlorhexidine rinse for an extra few weeks before removing the membrane. You probably will not lose all of the graft in this case, however you may not get the result you were hoping for. I believe this happened because you did not release the periosteum enough. Next time make sure you have absolutely tension free closure.
ttmillerjr
10/30/2011
You can see that the frenum is pulling on the flap when you pull the lip out. This is a test to see if you have tension free closure. I'd numb, remove the membrane, gently remove any granulating tissue under membrane and remove the top layer of the bone graft; until you are sure the graft is viable. Now you have another chance at closing tension free.
Dr.S.Lin
10/31/2011
Remove the membrane and irrigate the area well,if it's more than 3 weeks, you'll see tissue granulating under the membrane. The result may not be ideal, but you'll still get some growth. Yes, the problem was unable to get a tension free primary closure in this case.
TOBooth
10/31/2011
Hi,
maybe in the future use resorbable membrane.
In addition what prosthesis is over this augmentation?
Also if you are going to use a membrane you can use supporting tacks/ screws.
hope that helps , thi scase should resolved itself nicely make sure to wait at least 6/12 prirp to implant placement then additional augmentation may be need also what about 3mm 2 piece implanst or 3 m minis x4 / x3 ???
Antonio
10/31/2011
In my opinion, in absence of signs of infection, you could wait 2-3 weeks with application chlorexedine gel every 6 hours. In absence of infection, the new gingiva will cover the exposed membranes by creating new tissue.
In that case your regeneration may be successful
.
Dr.S.Lin
10/31/2011
Again ,take the membrane out,should slide out fairly easy. It will not be covered ! inform the patient to keep it clean with chlorohexidine rinse. Tissue should granulate under the membrane by now.
Dr. Omar Olalde
10/31/2011
Dear Dr. M, this is going to be solved as soon as you take out the membrane.
I can see you have no infection and the objective of the surgery was to increase the ridge volume, so I would wait 2 or 3 more weeks. But the exposure is going to be bigger each day. There is controversy in using Clorhexidine or not because it inhibits the collagen formation, so I don't use it when I use PTFE membranes. I use Triclosan, that's my own experience that I'm sharing.
Don't try to suture it.
Be ware of the pressure of the provitional prostheses.
When you take out the membrane it's going to be granulated in few days or maybe there is already epithelium under the membrane.
Good luck.
Dr. Omar Olalde
10/31/2011
And tell the patient that maybe you are going to do Bone Regeneration again when you place the implants.
Dr. David Goldberg
11/1/2011
1. Remove membrane
2. Degranulate inside of flaps to speed healing and remove any necrotic graft material
3. Gingival Grafts #'s 22 and 27
4. Consider a 6- unit bridge 22-27 (4 anterior implants are a tremendous challenge)
Dr Zaghi
11/1/2011
I have another suggestion for you. Extract the lower canines and place your implants immediately. In the anterior region use 3.5 mm wide implants and splint all of them together for the final prosthesis. This way you do not need to graft at all.
Bruce GKnecht
11/1/2011
This has happened to me more than once with this material. In fact you can almost expect this with this material.I would remove the membrane as was stated above. The tissue will cover the area in days. The tissue looks pink and I think you may be ok underneath. I would not disturb the graft underneath. This graft membrane is ok if it gets exposed not like Guidor used long ago.
baradds
11/1/2011
I have used cytoplast membranes extensively, unfortunately the tissue pull has exposed the membrane but as you will see the membrane exposure doesnt necessarily mean graft failure. I agree that you should leave it alone have the patient apply peridex to the area after all meals and before bedtime. You can remove the membrane after 20-30 days obviously the longer that stays the better.
In the future You should firstly extend your flap to the distal of the canine add verticles and make an incision releasing the flap in the periousteum so you have tension free closure. I would also recommend a titanium reinforced membrane and tacks so the membrane is more stabile.
Once you remove the membrane you will see that the bone is still there although you should wait about 6 months and take a scan to verify bone width. Sometimes you may have to do a secondary procedure or a procedure ie free gingival graft, or frenctomy or both prior to bone grafting.
norer
11/1/2011
Not one of the people who saw this case has used this membrane.
Do not worry this membrane is designed to stay un covered.
In day 21 to 30 this membrane begin to go out and you find down it a very good and health granular tissue.
You go in good way.
Only wait 6 weeks to see the results.
Do not do nothing with the soft tissue !!
HENOCA
David Mashburn
11/1/2011
The reason that we use non resorbable membranes is that they do not require primary closure. It looks as though the patient may be macerating the tissue with an interum prosthesis? The sutures come out in 10 days and the membrane in 4 weeks.If it has been close to 4weeks take it out. You should see epithelium under all that screwed up tissue. Have the pt leave the prosthesis out as much as possible. Relieve the prosthesis as much as you can over the site and line with a soft medicated liner (not a chairside soft reline). Cone beam at 6mo to see if you have enough bone to place an implant supported bridge.
Baker vinci
11/1/2011
Get more ce! If you are not aware of the fact that two mucosal edges cannot close primarily, without a vascularized bed, then you shouldn't be doing these cases yet. This is the premise of the guided membrane. I agree, use a resorbable membrane . I also agree with the suggestion of taking care of the frenum first. The frenectomy can't be done at the time of the graft, regardless of how you do them. You are going to find out just how hard it is to get good vertical augmentation in this case. You cannot make a silk purse from a sow's ear. Be prepared, unless you are adding volume via distraction or extraoral non-contaminated bone grafting, there are severe limitations to what you are trying to do . We are having some success with intraoral tenting and autogenous bone and or bmp. This is not a first timer case. Keep the area clean, with an antimicrobial( chlorohex.?????) and cross your fingers . You might get 3-4 mm of good bone. If you don't, start over ! Bv
Robert J. Miller
11/1/2011
This outcome belies a lack of surgical planning. There are generally two reasons for flap dehisence in these types of graft cases. First is an pronounced frenum pull. Second is lack of vestibular depth; more important when the adjacent tissue is highly mobile in function. With those two parameters present, you then add a non-expanded PTFE membrane onto which periosteum cannot adhere. You essentially guarantee this outcome. A frenectomy is necessary at a minimum. Better yet, an initial free gingival graft or vestibuloplasty will get you far greater mileage. Then use a resorbable collagen or PRF membrane so that you will get epithelialization over the defect within a short period of time rather than tissue retraction. Cytoplast membranes work best when the flap does not extend past the mucogingival junction.
RJM
Baker vinci
11/1/2011
David, in my hands , I use resorbable membranes without primary closure at least ten times a month , with excellent results. Unfortunately , I am running out of my membrane of choice and gore is going out of the membrane business. M. Block has suggested a Biomet membrane. I have asked multiple times on this site for any information regarding a membrane similar to the small rigid gore membrane, that has been discontinued . I bought there complete inventory and am down to about 15. I must assume the lack if response means that most readers don't use resorbables. If I am getting passive primary closure with periosteum to periosteum approximation, I don't use a membrane, in that I believe they are inhibitory . Bv
Sajjad A.Khan D.D.S,B.D.S
11/1/2011
Suggesting>
1 Chlorhexidne.12% rinse before and after meal
2 Frenectomy and support the flap with BSS without disturbing the membrane and graft.
3 Augmentin 875 po x bid x for ten days
4 Surgical guide or Fixed prosthesis like temp bridge to guard the site.
5 Please post your follow up case and treatment advice you followed
Juan collado dds
11/1/2011
Normal time to leave this membrane are 3 to 4 week,this is main reason because the tissue have been opened .it is time to remove the membrane and wait for it to complete the tissue closure and healing. This normal.
MarkHolloway
11/1/2011
I have only done 20 to 25 bone grafts and 20 implants. I sure enjoy these forums and have learned alot. The one thing I do not like though is when some know it all has to kick a guy who is sharing a failure or a problem. Everyone starts off with their first bone graft or implant. We are not all blessed with such genious and the ability to go all over the country taking 200 hours before we attempt a new procedure. You "know it alls" out there, be less judgemental and more understanding and lets help each other out with a little more empathy.
Baker vinci
11/1/2011
Mark , I'm not sure this is even a failure. I did see someone suggest he remove the necrotic bone and membrane. i'm not sure how this omniscient fellow knows this. The problem I see, is ,this practitioner doesnt know if what he has, is success or failure. Are you telling your patients that they are you 21st implant, when the formally trained surgeon down the street has placed thousands. I wish I had the time for two hundred hours of ce.. My ce , and a lot of other guys, falls into the realm of 5-6 years. Is there not enough work in your business, where you feel it's in the best interest of your patients to have a neophyte dabble around with implants. What happens , when you have a serious complication? Bv
David Morales Schwarz
11/2/2011
First of all, what kind of graft do you placed, particulated biomaterial or an autologous bone block? If you did the later you will have problems with graft exposure, if you placed particulated graft, althought you probably will loose some of the particles you placed there wouldnt be a serious issue.
Dense Ptfe membranes are designed to become exposed and to be removed after 3 to 4 weeks. As I can see in your case, there isnt signs of infection, therefore I would leave the membrane in place for about one week more. Removing such a membrane is avery easy task, you only have to pull slightly and the membrane will come out without any pain. After removing the membrane you will see granulation tissue covering the grafted area, dont even touch it, it will become reepithelized in a couple of weeks.
In my opinion youre not in trouble, dont worry and go on with your case.
Baker vinci
11/2/2011
Dr. Saghi, you are kidding correct? I am all about placing implants, but to suggest removing the two cornerstone teeth and place implants and a bridge. Someone go take this man's kit away! Why not just bridge from canine to canine and call it a day? What the f...... 20/20, 60 minutes,dateline and every other news station would be covering this industry, if that were exceptable." nothing replaces a tooth better than a natural tooth". The reason I didn't capitalize that statement is because I am quoting myself and don't believe I'm quote worthy. For heavens sake, get a cup of coffee before you respond. Bv
Baker vinci
11/2/2011
Maybe I need the coffee. Extract the canines and place 3.5 mm implants and use those as abutments. Is this patient an achondroplastic dwarf. You can't be serious . If I place an implant in a fresh canine sight it is never narrower than five mm and sometimes six. Would you " build your Peir abutement home on 3 inch I beams or 12 inch I beams"? Sorry for the harsh response, but you must have been up all night, putting someones face back together . Bv
scott
11/2/2011
I use these membranes all the time.
As stated these membranes are designed to be exposed.
I removed them 6 weeks after placement.
I have had amazing results with them.
Seems many of the doctors commenting are unfamiliar with this membrane.
Joseph Eastwood
3/4/2017
Please, expand on your statement of using a PTFE membrane exposed with great success.
It would be nice to know that one does not have to release a flap to gain primary closure, at times. Osteogenics for example who distributes Cytoplast membranes claims that they should be removed after three weeks. You, on the other hand, claim that you remove the membrane after six weeks with success.
Your reply would be greatly appreciated
Richard Hughes, DDS, FAAI
11/2/2011
A bridge from cuspid to cuspid is a rock solid treatment.
R Young
11/2/2011
I agree with scott. Continue your current hygiene recommendations and then remove the membrane at about 6 weeks. Granulation tissue will probably cover the graft and then let it heal.
Remove the frenum when you place implants if it looks like a problem at that point.
ali momen
11/2/2011
dear dr molares.thank you. iused FDBA mixed with autogenous bone and i fixed membrane with taqs & screws.
ali momen
11/2/2011
dear scott. howlong you will wait after membrane removal to insert implant if membrane exposed.
Joshua Shieh
11/2/2011
The material is engineered to withstand exposure.
NO TREATMENT IS REQUIRED.
Proper hygiene with 0.12% chlorhexidine mouthrinses may be recommended every 6 hours.
Wait for about 1 month before you proceed further.
Mark Cohen
11/2/2011
I use an Epigide membrane which I source from Reimser (Cerasorb co.). Thsi membrane is designed to be left open and have tissue grow over it. I like Mineross becacuse it handles well for me. It is corticocancellous so it serves a dual purpose as well. I have also had great luck with Dynoblast putty sourced from Salvin Dental. It stays where you put it and you can layer it. Expensive! I also don't disagree with the doctor who suggested the extraction of the cuspids as they look shaky and have no attached tissue anyway; cannot tell the whole story from this picture. Lastly, I disagree with the doctor who prescribed Augmentiin for 10 DAYS! I hope he has never had to take this med for 10 DAYS!
OMS resident
11/2/2011
Mark Holloway - You're correct: "Everyone starts off with their first bone graft or implant".
Some of us spend a lot of years in a controlled educational setting to create and refine surgical skills. Others do a week-end course in "bone grafts and implantology".
I guess I'm going to be hated for this one... Where's that coffee again?!?
Dr Zaghi
11/2/2011
Dr Baker Vinci,
I think you are the one who needs to take a cup of coffee before responding not me. Fist of all I suggested you place 3.5mm wide by 10mm or 13 mm length implants in the edentulous areas WITHOUT EVEN HAVING TO PUT THE PATIENT THROUGH THIS PAIN AND AGNOY OF GRAFTING in the first place. Then, you can place 5 x 13 or wider implants in the canines sites.
Second, even though we haven't seen the xrays, the canines obviously have periodontal issues. So for those folks who suggested to do a bridge on those teeth, I suggest they go and review their dental school text books.
Dr.B
11/2/2011
Someone recommended extracting the canines and immediate implants. I had a similar case where I extracted the canines and was planning on immediate implants, however after the extraction I noted there was no buccal plate. I had to delay implant placement. I learned a valuable lesson. While I think it's a good idea, one should beware of the possibility of losing the buccal plate. Recently I have used the Straumann Roxolid implant which is 50% zirconia and is advertised as an implant that can be used in compromised ridge situations such as this case. I have used it to replace premolars in a case where the patient absolutely refused any bone grafting whatsoever. Has anyone had any experience with it?
TOBooth
11/2/2011
wowzers ego's are flying around everywhere.
this guy only wanted an answer to his question.
If in doubt think simple.
D'ont prep the 3's!!! old school however, perio do respond well to salvage bridgework.
Immediates-bad look up Botticelli paper.
5mm /6mm implants in a lower 3 spot you guys are crazy!!!!
CE and major complications, come on its not micro brain surgery apply basic principles
implants in 2's-augment any deficiencies place in correct plane bucco lingually depth ;expose slightly from the lingual ; custom abutments bridgework-DONE.
Baker vinci
11/2/2011
Dr. Zaghi, my regrets. Yes my response was precaffiene .so I take back the suggestion of you putting 3.5 mm implants in the canine sights,but stand strong , when i express opposition to removing canines. Are you an endo or perio doctor? If you are either , are you just throwing your hands up at chance of saving what may be perfectly good body parts? Are teeth just"White Lesions" to you? If this patient comes to your office and you were to have no more information than you have, extraction and implants would be your first suggestion? If you were in an examination room taking an oral board exam, you would be going back home to prepare for your second or third try. Maybe your not interested in my opinion or with standard of care medicine, but this form of treatment is a conflict of interest, regardless of what you are. Why just 3.5 mm? What if his ridge width could accomadate 4.3 or 4.5 mm fixtures? Getting my evening cup of coffee! Bv
Baker vinci
11/2/2011
Tobooth, this has nothing to do with ego's. But when a neophyte is asking a question about something he is clearly unfamiliar with, then it is our obligation to give him sound advice. If anyone is taking this stuff personally then go see someone and "share your feelings with the group ". If this guy is taking this advice , he has removed the membrane and the bone, which may have been perfectly good , and removed two lower canines and turned this patient into a true "dental cripple". What next just complete edentulation and nerve lateraliztions . What gives , with the suggestion that bone grafting causes so much pain. What am I missing? Am I giving my patients too much pain medicine? The only time a patient truly complains of pain in my practice is after a large anterior hip harvest or a rib/clavicle graft, for tmj reconstruction. Sorry ,for calling people out, but this guy is asking for help and it seems some of the respondents have given some sound advice. Bv
alper
11/2/2011
Cytoplast membranes can be left exposed therefore you dont need to do anything. Just tell your patient to use listerine and clean the exposed area with cotton pellet till healing. After 3 or 4 weeks you will see that soft tissue will completely close the inner part of the membrane. After that you can remove the membrane. We have used this d-PTFE Cytoplast membrane for case series and I purposely leave it exposed for 4 or 6 weeks. It really works..Good luck
Robert J. Miller
11/2/2011
Yes, cytoplast membranes ARE designed to be exposed at time of placement. But this is no excuse for poor surgical planning or pushing the envelope in a large graft case like this. If you go to the cytoplast website, or watch clinicans lecturing for the company, virtually every case you see is single tooth site where the mucogingival junction is stable. This will prevent substantive flap retraction as demonstrated in this case. What we need here is a little more critical thinking about the consequences these materials have post-surgery. Other than exclusion of fibroblasts, there is little else that is biologic about non-expanded PTFE. Resorbable collagen membranes also exclude fibroblasts but have a positive effect on periosteum and allow epithelialization over the graft site. PRF membranes also do the same but add growth factors that enhance early angiogenesis and have an anti-infective capacity from viable leukocytes (at a cost of $5.00 per membrane). Understand the limitations of each protocol and make clinical decisions that reflect the biologic imperative of each individual case. You will reduce untoward events such as the one posted here and dramatically enhance surgical wound healing and final prognosis.
RJM
Michel P. Jazzar
11/3/2011
L-PRF Membrane: if you follow the protocole and its indications, you get very good results. Good luck.
Baker vinci
11/3/2011
Dr. Jazzar, what is the company name?Bv
Robert J. Miller
11/3/2011
The PRF System in the US is sold by Intra-Lock International. They also have courses to show how the membranes are fabricated and cases to show both soft and hard tissue applications.
RJM
TOBooth
11/3/2011
clearly nothing to do with it!!!!
timel
11/3/2011
Resorbable collagen membranes are the way to go. They don't require primary closure (at least the one I use) and they are user and pt friendly. There are numerous suppliers and readily available.
Baker vinci
11/4/2011
Tobooth, your exactly right , we don't need no stinking ce.. Complications, smoplications, that's just nonsense. You don't have enough time in a day, to review all of the things I have removed, repaired,transplanted,and admitted because some guy was operating with that mentality. It's not" micro- neuro", but it is just as important when your on the recieving end. I have changed my philosophy, big time, since entering the arena. I know that everyone is going to try it, so I am going to do my part to help. I have talked two patients out of taking legal action against nontrained practitioners, in the last four weeks. One to the tune of doing the case, probono, and I will say they would have fair cases,with a jury of their peers. By the way, forums are designed to spark, creative thinking and or controversy at times. He got his answer. Bv
Richard Hughes, DDS, FAAI
11/4/2011
In the USA we have several experts in bone physiology and grafting.
They are Eugene Roberts, Maurice Valen, Andy Tofe, Pikos and Robert Miller. I think it would be neat to get them together and learn from them. We all would be better docs from this!
Baker vinci
11/4/2011
I agree dr. Hughes . Just getting visual on that . Am I seeing "eyes wide shut" or " blazing saddles". Would have to put a few more panel members . I would be in the audience , at the back row. Good weekend all. Go honey badger????bv
dr.t
11/4/2011
[quote]Dr. David Goldberg says:
November 1, 2011 at 3:35 pm
4. Consider a 6- unit bridge 22-27 (4 anterior implants are a tremendous challenge)[/quote]
Please, please, PLEASE do not do a 6 unit bridge. This woman is 30 years old. Why did she lose the teeth in the first place? My guess is Perio, since you can see the roots of the canines already. If she couldn't keep the anteriors clean before, she'll NEVER clean under a bridge, and she'll end up losing those teeth too. Right now the canines look like virgin/uncut teeth. Why cut away healthy enamel? Its unethical.
A removable or implants is the only way to go.
Baker vinci
11/4/2011
Dr. T , welcome to the site ! Finally ,someone remembers what we are supposed to be doing . You don't need to be a surgeon or a phd in bone biology to understand some of these PRINCIPALS. I agree, removing good body parts without informing the patient, fully of the destruction associated with taking out canines in an a patient that has already neglected teeth is absurd. In this specific case,we don't know if this a defect left after a rim resection or management of bronj.. I discourage splinting at all cost. Just my opinion. Bv
John Kong, DDS
11/4/2011
Nicely put RJ Miller. There are many opinions and jibberish here, some good ones and many retarded ones, 'specialists' included. For those recommending exo of the canines, you cannot make a proper prognosis without x-rays. Who cares if you can see part of the root? For all we know the roots can be 25mm long!
John Kong, DDS
11/4/2011
Nicely put RJ Miller. There are many opinions and jibberish here, some good ones, some funny as hell and many retarded ones, know-it-all 'specialists' included. For those recommending exo of the canines, you cannot make a proper prognosis without x-rays. Who cares if you can see part of the root? For all we know the roots could be 30 mm long!
Baker vinci
11/4/2011
Dr.B , as you can see ,I am not at all for removing the canines in this scenario,but for the one you mention ,it is my suggestion,that the next time you run into a fx buccal plate when trying to place an immediate implant, go ahead and place it as long as the other walls are in tact. A good membrane and some autogenous bone will grow a buccal plate. The membrane will be tented by the unfractured portion as well as the mesial buccal and distal buccal portion. Bv
Dr.B
11/5/2011
Thanks BV, I did consider that but felt that the case was too compromised at the time. As a famous implant surgeon is known to say: "one miracle at a time". I decided to graft prior to implant placement. Although I am experienced in implants I certainly learned a lesson from that case. Looking back, I would have not extracted the canines, or I would have at least ordered a CBCT to view the width of the buccal plate. I believe that most of us in this forum if not all have the patients' best interest in mind. Although sometimes we may push the envelope with good intentions to save the patient time and money we may run into unexpected situations. When that happens I think it's important to step back and re-assess and fix the situation, even if it will cost us our time and money.
Baker vinci
11/5/2011
Dr. B , pave the way and get a scanner, now. I purchased mine , after spending years saying , I don't need a ct to place an implant. I bought mine with the intention of having this important tool, readily available , in that the technology has been standard of care in my practice since the pacs system was invented in the late eighties. Even with doing, two or three free, a week , it has paid for itself in multiples, in just 6 or 7 months. It allows me to avoid operating, when it's unnecessary and it makes all surgeries safer, more predictable and on average ,cuts the surgery time in half , in most cases. Bv
Albert Hall
11/6/2011
There are resorbable collagen membranes in the market with better behavior for this cases, ptfe membranes are no longer the treatment choice,since we all know what happened with Gore-Tex membranes (extensively proved).Bio-Gide from Gesitlich should work much better.
It came to my attention why you mixed autogenous bone graft with cadaver bone material? Both materials in case of any exposure will get infected very quick.Definitively in cases like this and many others, we need to use proven materials and not rely on manufacturers trying to compete with products at a lower priceing.
Baker vinci
11/6/2011
Dr. Hall, enlighten me please ? I'm embarrassed to say I'm out of the loop as to why gore is out of the membrane business. You are the first to directly respond to my question. I can't imagine a better membrane, than the small gore, that I am almost out of. This membrane that you propose as a substitute ,is as stiff as the rigid small? Eagerly awaiting your reply. Thanks, bv
Idt
11/6/2011
I couldn't disagree more with dr hall. Bio guide is a nice membrane but there are newer better membranes like vitala, curve, epiguide. Kls Martin makes a nice kit but pricey.Â
Cytoplast membranes in my hands are wonderful. I prefer to use the titanium reinforced ones. I recommend tacking them down. Getting passive primary closure and using internal horizontal mattress sutures to prevent opening.Â
In this case you used the cytoplast txt without tackIng which has memory and will put tension on the tissue and failed to reposition the frenum prior to surgery. This case has a strong muscle pull and shallow vestibule. You needed a more remote flap design and better releasing incisions.Â
I would also incorporate either ct graft or dermis over the membrane.Â
For better instruction refer to dr fuggazzatto book or take some ce with osteogenics.Â
That being said you have the protection of the cytoplast in this case. Use it to your advantage. As long as there is no pus from the area leave for 6 weeks total allowing tissue to heal. Then remove and get really good release passive closure.Put some puros dermis prior to closing over the graft. Do not let it get exposed. Get a ct in 4 months and reevaluate. Will probably need additional graft hopefully you can do at time of implant placement.Â
Idt
11/6/2011
BV- gore is out of the dental buisness. They make too much money with gortex products and find the dental industry unproductive. Similarly HP no longer makes personal computers as the margin of profit is small compared to their enterprise division. Thus these small profit margins bring down the stock. Plus gore is penetrable as it is e-ptfe. Cytoplast is d-ptfe and doesn't allow bacterial penetration when used correctly. It is considered the state of the art membrane not as dr hall referred to as "no longer he treatment of choice". As opposed to your faviorite gore membrane it has proven science that it allows penetration. I strongly suggest you look into these membranes.
Baker vinci
11/6/2011
Idt, I believe it is the penetration that makes it work. I have had but a single infection with the small gore and most of the graft survived. Clinically, when I see the membrane starting to break down at 3-4 weeks a protective coagulum has already encompassed the bone graft and my results have been better than satisfactory. Granted I only use this one for single or double tooth ridge preservations, but I place my implants at 3 months , if I didn't place it at the time of extraction. Occasionally I'll have to add a small amount of Bone around the implant at 3 months. The reason I like that small gore so much , is because it's very rigid and easy to handle. Fortunately gore is still selling the suture. Bv
Robert J. Miller
11/6/2011
I'm curious as to why you would classify Cytoplast as a "state-of-the-art" membrane. Non-expanded PTFE membranes have been available for well over a decade from other manufacturers. They went nowhere until a dentist decided to form his own company, come up with a flashy new name, and then employ very visible clinicians to help market an old technology. It never took off years ago and, quite frankly, there is no biologic argument to make it take off now. But I guess that this is the power of marketing.
RJM
Baker vinci
11/7/2011
Robert, I think you need to readdress the response to the original question. There is no way he is going to get primary closure without some breakdown, regardless of what he has under that membrane. Yes, the frenum is exacerbating the degree of dehiscence and the lack of vestibular depth doesn't help. Undermining and attempting primary closure is going to shallow the vestibule even more. I'm doing( have done, several) two cases in the next two weeks, with a similar scenario. One will get reamed femur bone placed extraorally with small midface plates placed over the top, to maintain space. The other is getting a vestibular incision , with autogenuos graft material and probably a filler. I will have and keep primary closure on these two cases. one Patient had finally passed the nicotine screening test, as she was not being operated by me, otherwise. This was after I forced her to get 2nd and 3rd opinions. This doctor asking the question needs to appreciate the limitations associated with these cases. Are you getting infections with these procedures? Also, please disregard any suggestions of attempting to suture this inflammed tissue, as it will hold stitch about as well as a squamous cell carcinoma.( that was directed to another suggestion) . Again these are my little personal suggestions and rhetorts(is this a word?) bv
Idt
11/7/2011
Over the next year or do you will see several new studies with infuse and cytoplast. Originally thought that infuse needed to be used with penetrable mesh now further studies are confirming as periosteum is the source of your inflammatory cells. The results I'm personally seeing are amazing. 4-6mm vertical hight with similar density to ramus blocks. The old nonexpanded ptfe were not textured. They did take an old idea but enhanced it. LED technology has been around over 20 years before someone figured out how to make it work for TV's and now we all have these in our living rooms. I use several types of membranes as discribed previously my point was this case did not have to be done with bio guide. We can all use what we feel comfortable using as long as we respect the environment for them to work.
Baker vinci
11/7/2011
They are just now confirming that the periosteum is the source. Bruce Epker , RV walker, bill bell et. All have preached this for decades and this might be why Alan herford is at the forefront of publishing this stuff. Granted some may have been anecdote, but the rhesus monkey studies( the acid test of oral surgery), did give us some scientific enlightenment with regard to the above. This is why the maintained volume of an intact sinus grows bone with no graft material. This is also why the 15 year old female , with the desmoplastic amelo and inferior border preservation procedure, grew bone with no maintained space. You will never convince me that that appropriately placed Caldwell luc window needs a membrane, if the periosteum is In tact. Please, no one get their thongs in a wad, I am essentially agreeing . If ,it at all matters. Bv
idt
11/7/2011
BV-very true. I’m conducting a study in mexico that was previously done in Brazil and published in Implant Dentistry amongst other locations of just PRF in lat windows. The trephined bone is not as dense as you would expect however we are seeing a lot more haversion systems. Seems the bone just needs a little more time to mature. I believe this is the future. Stem cells etc..
Robert J. Miller
11/7/2011
B.V., this is exactly why I suggested a pre-bone graft free gingival graft with frenectomy or vestibuloplasty. IDT, can't quite grasp your logic. Teflon will have the same effect, textured or not; no cell adhesion can take place. If we do what B.V. has suggested and go back to the original question (photo), we see that even with a textured Cytoplast membrane you had unacceptable tissue retraction. With regard to rhBMP, the findings of all of my colleagues suggest that while you get a significant increase in volume, in every case without exception the bone is rather immature and can be pierced with an elevator. The thing you have neglected to post is how long you allowed the bone to heal prior to implant placement. At 8 months or beyond, you can expect any of these graft materials to have similar results. I have used virtually every graft and membrane du jour and have finally settled on biologics. If you can't beat Mother Nature, then use her to your advantage.
RJM
Baker vinci
11/7/2011
Robert, absolutely agree with addressing frenum pre- graft. Also was excited at first suggestion of mucosal tissue expansion, as it has done wonders for bad burns and even refractory keloids on the face and neck. Just as soon as I considered trying it, I got shot down by some respected colleques and I guess ,rightfully so, because I haven't heard much about is since. Seems to make good sense however, but non the less vestibular or trans- neck seems to do quite well as long as volume is maintained, somehow. Porex is apparently on the cusp of steriolith. Fabricated system that acts like meshes, that don't require removal. The case presented may have been a great case for sandwich or visor procedure. Bv
Idt
11/7/2011
The newer technique for infuse involves wrapping the infused btcp with graft material similar to sushi rolls. Allow 6 months bone is hard as a rock although this is off label at this time. Frecnectomy with sufficient release and dermis over the graft should be enough. Why torture the pt with fgg unless necessary. I used to do that all the time prior to learning rotated pedicle flaps and how to obtain primary closure. If you have no vestbule than I agree fgg is appropriate however we don't have preop photos here so we cannot say. Btw if you love mother nature check out the vitala membrane. Much easier to use than bio guide.
peter fairbairn
11/8/2011
Does anyone know about what happened to the reports ( IHT in July ) the suppresion of of research on serious side effects of BMPs by the manufacturer . Using it "off licence" could have future leagl issues.
Idt
11/8/2011
Not sure. All my experiences have been in Mexico where it is legal.
Richard Hughes, DDS, FAAI
11/8/2011
Baob Miller, I agree with you 100%. I know autogenous is the best and use it when I can. That said, I have histology studies of my specimens performed at VCU Oral Path Lab that show that Osteogen will turnover and yield 90% lamellar bone at 6months. 90% isnas aboutnas good as it gets for a synthetic.
Baker vinci
11/8/2011
I believe the use of bmp is on label for ridge preservation grafting as well as sinus lifting, unless the ridge defect is a result of tumor ablation. Regardless "off label" is relative standard of care. The FDA is just the "man in the suit that bought a new car". Again reference "low spark". No music aficionados here? Bv
Gregori M. Kurtzman, DDS,
11/10/2011
Unfortunately a common issue with non resorbable membranes and not a big issue at this point. The tissue at the margin are non inflammed and it will be impossible to get primary closure now. Have the patient use CHX rinses and allow it to granulate over will take time as gingival tissue only grows at half a mm a day. Once covered over you can address tissue thickness when the membrane is removed (after a few weeks once tissue has covered over the site). If need be a connective tissue graft can be done then.
Baker vinci
11/12/2011
Peter, I have heard from some pretty powerful resources that some of the ortho studies on bmp were significantly misrepresented. I hope what I'm hearing is false, in that bmp's are one of the most published items, with regard to large recon. cases in the maxillofacial lit. ,both in the USA and internationally. I personally, am a stem cell advocate, and vote on the starboard side. I will not even attempt to start a discussion about this. Sorry for mixing politics with real science. Bv
Baker vinci
11/12/2011
Additionally, the only paper I have personally seen regarding any complication ; is the report of a death after cervical spinal fusion surgery, that was a result of airway embarrassment, from oedema . If you have used the product for large cases you know that the majority of patients have firm swelling, that can be somewhat alarming. Some patients on the other hand don't swell as much. It is the (swelling) recruitment , that is the catalysts for the success of this product. I med. searched before this response and did not see any other complication. I personally, think it is going to be a great product one day, but feel like the hype is slightly overshot. Bv
Baker vinci
11/13/2011
Robert, seems like you have run the gambit on membranes. I haven't , in that I'm not an academic and since my discontinuation of nonresorbables, the gore has served me well. Of all the membranes mentioned , which one maintains it's stiffness , even once saturated with fluids from the surgical sight? I do not tack membranes, in that if I am in that situation , I will use a metal crib/mesh. I feel like creating enough exposure to place a tack , is robbing Peter to pay Paul. Not interested in discussion about that, but if you guys are ,let it rip. Patiently awaiting your response. Bv
Elie
11/14/2011
Non Absorbable PTFE membranes are used in case we can't have a primary closure tension free flap, to cover and protect the bone graft.
Usually,in a case like that , I use the double membrane technique (collagene membrane + PTFE membrane)
Their function is to stay exposed during 3 weeks.
The criss-cross PTFE sutures are removed at 10 or 15 days.
Remove the PTFE membranes using a tissus plier , no need to anesthetise the patient.
CHX mouth rinses are mandatory during one month
Robert J. Miller
11/14/2011
The extended resorption time membranes are generally more stiff. They can either be cross-linked Type I bovine achilles tendon or a non-crossed linked collagen infused with polylactic acid (PLA). However, once they are wet, they all deform to some degree. If you dislike tacking them with titanium tacks, try using resorbable PLA tacks. No secondary surgery is necessary for removal. If you are looking for no movement and absolute control over volume, there is still no substitute for Ti Mesh. There are some new technologies coming to us from France, which includes a CAD based custom Zirconium cage fabricated from a rapid prototyped model or from a virtual model with openings at crest for placement of graft material.
RJM
Baker vinci
11/14/2011
I'll probably not be convinced that tacking is at all necessary, in my hands, when I'm using these small membranes. I have used some resorbable hardware in the infant synostosis patient and growing young jaw fractures. Am I" SOL", when it comes to replacing this piece of my armeterium . Just got a few samples of the Biomet . Will give them a go. Maybe I'll start up my own company, with the
material in the small gore. "Vinci Guided Regenerative". Nice ring to it, eh? Bv
Baker vinci
11/15/2011
Well, since you addressed the of subject issue, I will give you my reasoning behind my refractory attitude towards tacking. As I mentioned before; tacking requires obtaining greater access, subsequently robbing the graft bed of the highest possible nutrient source. Secondly, with my limited experience of multiple types of membranes, I have found that placing holes in the membrane( four ), decreases the breakdown time and potentiates tears in the material. I have no problems keeping membranes in place, in that I take large bites with a premium suture and am "a Nazi" , with regards to post op care. Oops, sometimes I forget the site is international. Tough doo doo! Bv
Baker vinci
11/15/2011
Off subject
OMS resident
11/15/2011
BV - you mentioned that you've used resorbable hardware in some infant and growing cases. Have you ever seen any sterile abscesses related to the (resorption of the ) hardware?
Baker vinci
11/15/2011
No ,I haven't but it's been a while ago. I have heard of such, Just as you might get with subcuticular chromic. I am by no means, an expert in this, in that I haven't used the resorbable systems more than 15-20 times. I'm still a titanium guy ,with the rare exception. Bv
J. Perry
11/16/2011
Dr. M. I would like to see or read what the end result in healing in this case and which recommendations were followed? Thanks
Johnny Knox
12/19/2011
Resorbable mesh would work better
Matthew
4/6/2012
looks fine.
leave in 2 to 3 more weeks.
remove.
allow to granulate.
implants in 5 to 6 months.
peridex.