Mucositis or peri-implantitis?
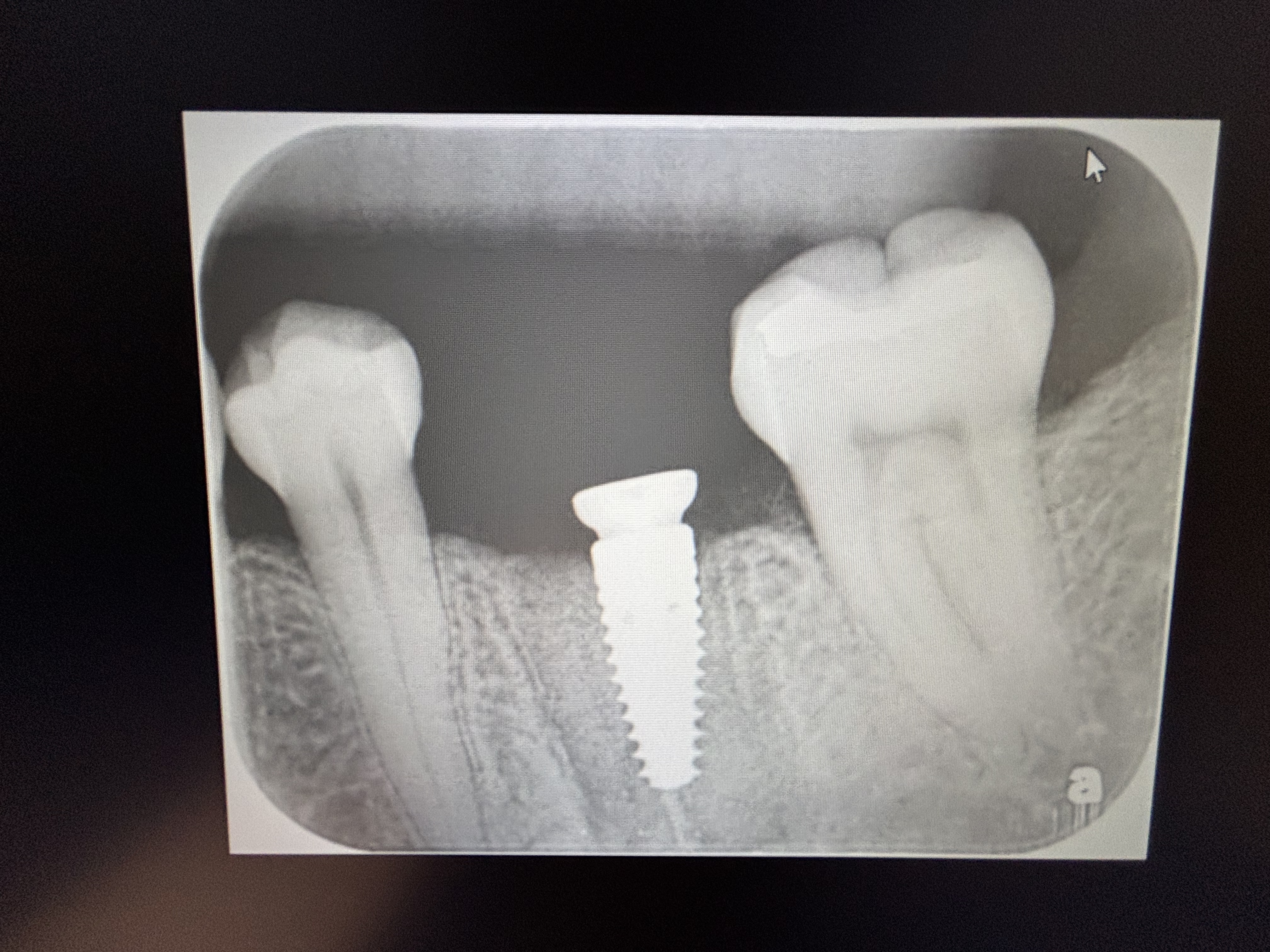
This patient had 2 implants placed by another dentist approximately 5 years ago. She recently developed a small sinus tract adjacent to one of the implants. Does this look like mucositis or peri-implantitis? How can I determine what is going on here? What treatment protocol would you recommend?
 Sinus buccal to crown
Sinus buccal to crown radiograph with gp point inserted in sinus
radiograph with gp point inserted in sinus radiograph with gp point inserted in sinus
radiograph with gp point inserted in sinus
19 Comments on Mucositis or peri-implantitis?
New comments are currently closed for this post.
CRS
1/11/2013
This looks like mucositis with early peri-implant its due to bone loss at the first thread. You could start with arrestin and follow up with flap debridement, detox the implant surface maybe GBR or graft. What really makes me nervous is the occlusion. The class II overbite with the lower teeth banging into the implants and the pink porcelain which leads me to believe that the bone loss was ongoing with the natural teeth. I'd think about restoring the posterior vertical since the occlusion it hard on these implants. I'm a surgeon so I can only recognize not the best to advise. Perhaps referral for treatment for the peri-implantitis this a headache that you inherited due to tunnel vision on the anterior implants. Don't want to judge since I was not present at the treatment planning. Nice case for discussion. Good post. Also this time frame is correct, we usually start seeing these problems around 5-8 years post implant placement.
Leal
1/11/2013
In a 1 second view the x-ray looks really nice, everything looks really nice, however this is in a 2-dimension perspective.
What's the buccal perio probing like?
Probably a lot of buccal bone resorption lead to this, like ~10 threads exposed to buccal gum. Flapless surgery (incorrect placement), no respect to the minimum buccal bone width, etc. are just a few possibilities.
CRS
1/11/2013
Very good point if that's the case it will be determined at flap elevation implants may need removal and the ridge grafted . I always like to see what I 'm putting the implant into, I only go flapless if I 'm CT guided. Excellent point.
Peter Fairbairn
1/11/2013
Hi Yes could be a good discussion , but Implants placed a bit deep for this type of implant and hence bone to first thread hwere it still is after 5 years . So a goood case loooks fine just a mucositis and to be treated with improved OH and CHX . This patient has a poor oral situation and things do not change in their lives .
But the implants look fine , bone to the first thread .
Buccal perio probing would be helpful as said.
In this age of crestal and sub crestal placement some surgeons fail to see the different protocols that strangely have stood the test on time
Peter
CRS
1/11/2013
Not sure how the implants were placed I would guess crestal since there is pink porcelain present. I agree that die back seen to first thread is fine seen with deep placement and biological width. However some surgeons scallop the anterior bone. Main point is that mucositis can advanced to peri-implantitis and since previous films from placement and follow up not posted placement is speculative. I like your perspective, I would start with Peridex, then Arrestin, then a flap debridement depending on response. The poster needs to decide how far they want to go in the maintenance schedule.
Peter Fairbairn
1/11/2013
Hi CRS , yes when I enlarged the photos could see the micro theads so yes a small amount of loss ......... but after 5 years that is not bad and no-one has died.
Peter
CRS
1/11/2013
I like your perspective, very wise!
greg steiner
1/11/2013
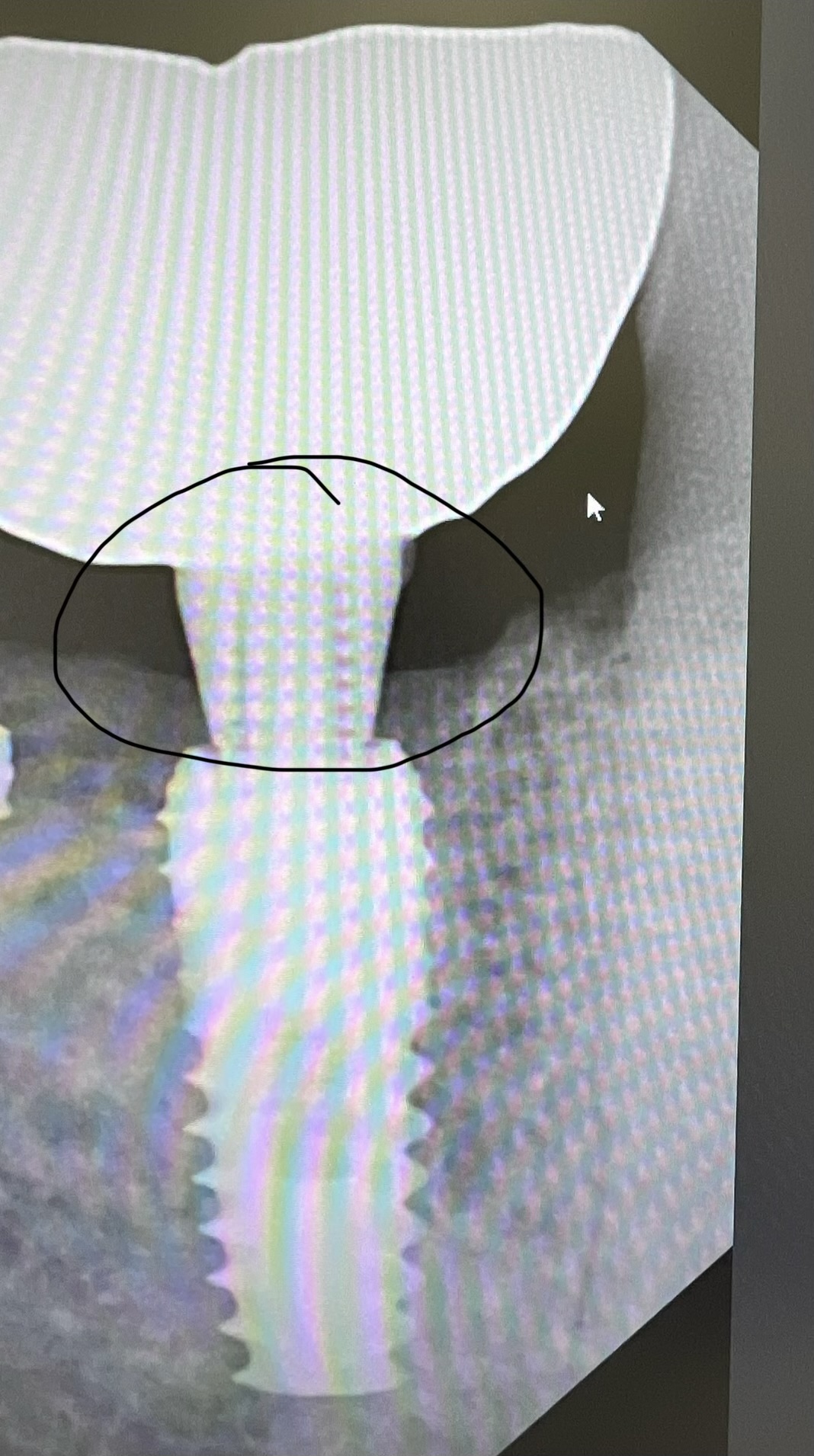
In my opinion the gutta percha hit the implant and was deflected to the mesial rather than following the lesion toward the apex. I wager the bone loss is to the last thread before the taper. I would anesthetize and explore with a probe in the fistula before embarking on a treatment plan. Greg Steiner Steiner Laboratories
Leal
1/11/2013
Agree.
Richard Hughes, DDS, FAAI
1/12/2013
Drs Leal, Greg, CRS and Peter: you all have made valid points. I hope there are more people reading your advice.
The lateral incisor has a marination issue on the mesial. In my opinion, these cases that present with inadequate posterior occlusal support, are poor candidates for implants.
I would flap, degranulate and detox the implants, put the patient on peridex and monitor. I would like to see the patient receive more implants and fixed treatment to establish a balanced occlusion.
Robert J. Miller
1/12/2013
Are these Nobel Replace Select implants or a clone?
Richard Hughes, DDS, FAAI
1/13/2013
Correction, the lateral has a margination issue.
Oleg amayev
1/13/2013
Where is the sinus??? I would flap it, debride, arrestin, close the flap.
Alex Zavyalov
1/14/2013
The problem is much wider - a traumatic occlusion is/will be the cause of gum and bone tissue destruction, because of posterior teeth absence and overloading of the frontal area.
David Robinson
1/15/2013
rather than diving in and possibly needlessly causing damage , seems sensible to follow Peters approach with OHIO etc , . chances are this is sufficient but if sinus persists more than 6 mths , then consider other options . it may convert to a fibrous healing nodule.
bviously improving posterior occlusal support may help long term but bone level around implants after 5 yrs seems quite good on X-ray.
michael w johnson dds ms
1/15/2013
This most likely is a sinus tract to the abutment- implant junction. I have seen several fistulas over the years that most likely is caused by micromovement at this junction. The implant radiographic bone level looks fine, bone loss to the first thread is an accepted norm with flat top implant designs so I don't think flapping, probing etc. is necessary in the absence of gingival inflamation (this is a fistula, not inflammation) unless residual cement is suspected as the cause of the fistula.
Check for micromovement of the implant crown which could cause percolating of bacteria at the microgap. This may be especially true due to lack of posterior occlusion as alluded to earlier. Treatment is tough. Once a fistula epithelializes it never heals and is nearly impossible to excise due to the flimsy nature of the tissue.
Anitbiotics can help but probably not heal the stoma. A way to minimize the risk of microgap movement and microleakage is to use an implant with a conical abutment connection like the Astra or Straumann bone level implant systems (there are many other good systems that use this connection too).
wmcgonigle
1/16/2013
Check for excess cement when raising a flap. How about also placing an implant in # 10 area? However occlusion and posterior support is crucial.
Juan Rumeu
1/19/2013
I agree with Michael johnson. This is the typical case of an abutment infection. I would not do a surgery by no maens. Just remove the crown + remove the abutment + clean it up and place terramicine ofphtalmic cream inside before you place it back again. Problem solved and the fistula will go away by itself.
Adam
2/26/2013
The patient has limited posterior support/bite and when incising would likely only occlude on the implants on 8 and 9. The bone loss around the implants looks like cratering from occlusal overload. So, whatever else is happening physiologically, I would plan on addressing the occlusal aspects as part of the treatment plan so you're not just treating symptoms of the problem. My two cents.