Patient on Aledronic acid and Methotrexate: Risks of complications?
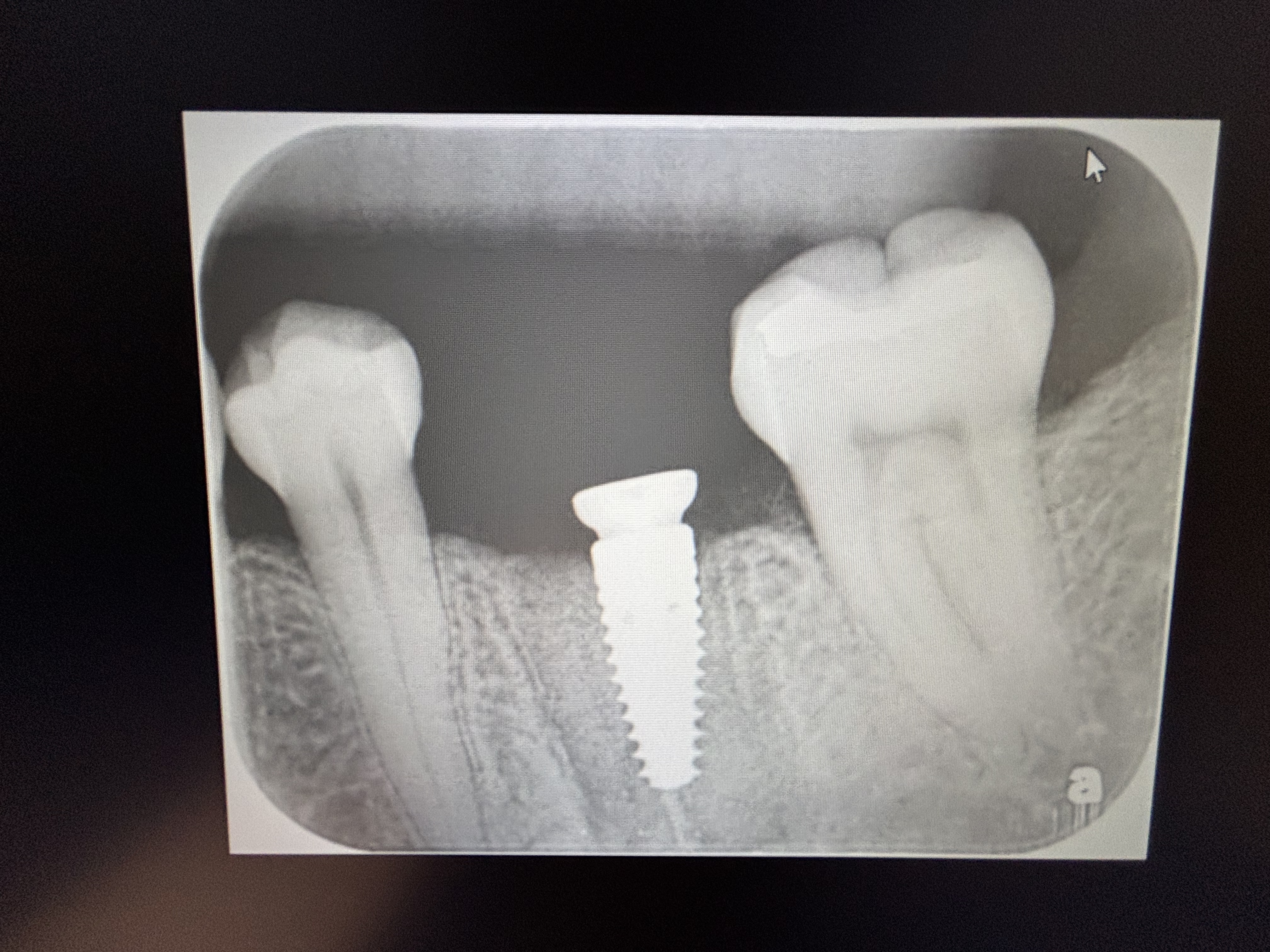
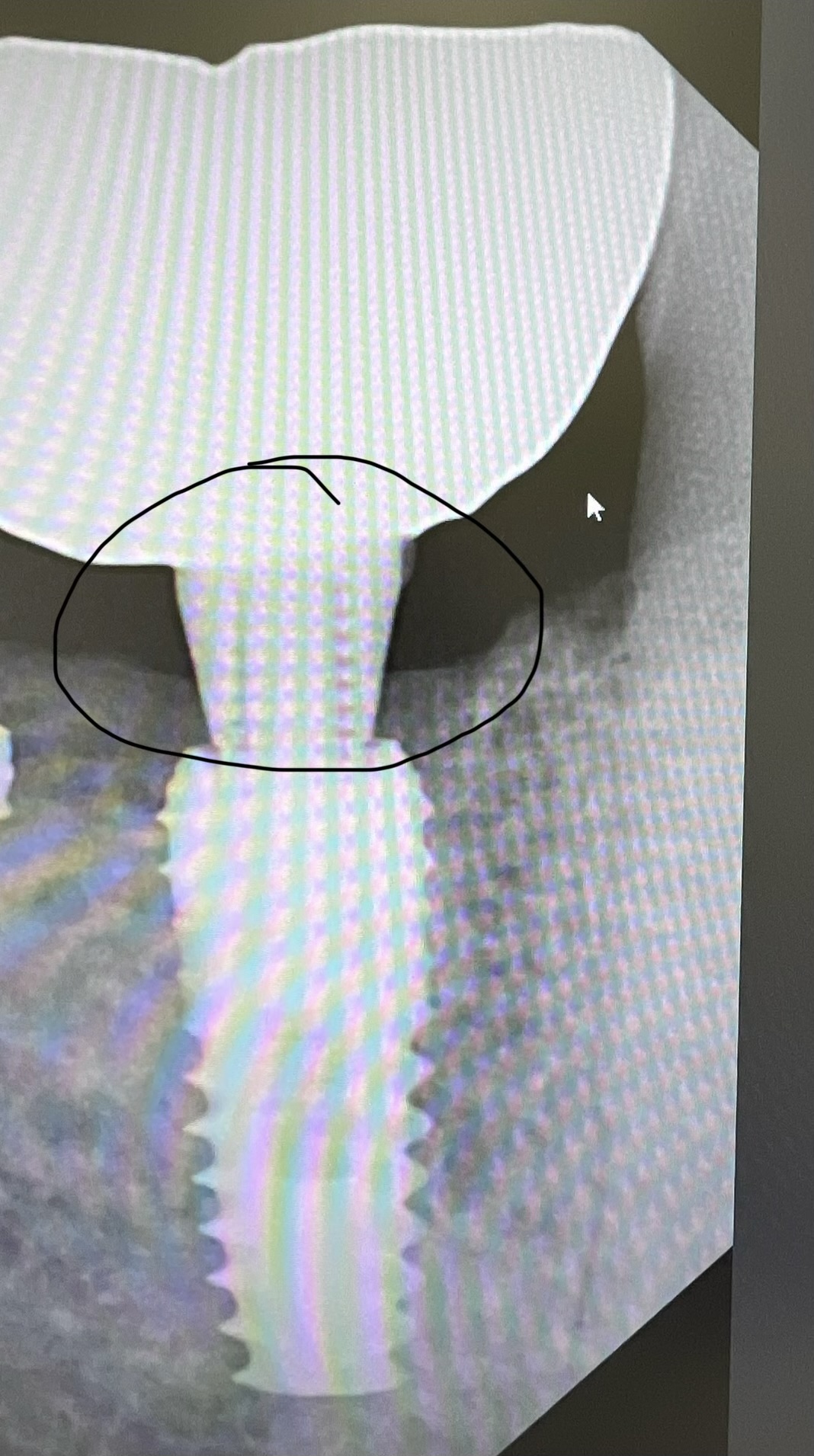
I have a 68 year old female non-smoker who is taking alendronate acid 70mg every week (a bisphosphonate drug used for osteoporosis sold as Fosamax by Merck) and is also taking methotrexate (an antimetabolite and antifolate drug used in treatment of cancer, autoimmune diseases). I would like to place dental implants in her maxillary second molar region. I think the general consensus seems to be that alendronate acid on its own does not present a problem, but she is also on Methotrexate. What are the risks of complications for the alendronate and the methotrexate? Would not touch her if on prednisolone, but what is the consensus about Methotrexate?
11 Comments on Patient on Aledronic acid and Methotrexate: Risks of complications?
New comments are currently closed for this post.
CRS
7/21/2013
Discuss with her physician why she is on these meds, duration of treatment and prognosis. Then have him clear he for your recommended dental treatment. There are numerous BRONJ resources inline of course I'm partial to the Marx protocol and AAOMS protocols since oral surgeons usually manage this and are your backup.Most of the protocols copy this. Adequate patient information and consent. The Bisphosphinates are an unpredictable animal, I've seen problems ten years down the line and have also had successful implants placed in these patients. The drugs have a very long half life and we just don't know how to predict who and how severely the bone will be affected. Don't put confidence in a test or an article read in a ADA journal. Osteointegration is especially unpredictable in these patients so don't promise something you are not sure of. Combining this issue with Methotrexate adds another potential problem which her MD and a literature search will help. Remember, dental implants are elective and the risk benefit ratio need always be considered. Theses are my recommendations, and your welcome!
FF Jr.
7/23/2013
I personally would not do it for a few reasons. As stated above, Fosamax and other oral bisphosphonates can be very unpredictable when it comes to primary stabilization and long term stabilization of implants. Secondly, Methotrexate is a medication which is usually used in severe cases of certain disease processes and can cause patients to bleed and also eventually become immunocompromised. You must find out why she is on both of these drugs from her physician. Many times implants are not very successful in immunocompromised patients. Thirdly, you are talking about the upper second molar area for your implants. This area has the least amount of dense bone and is really an elective place to put an implant. Most do well with replacements to the first molar area. That is why I would probably leave well enough alone.
Vipul G Shukla
7/23/2013
It is well documented in most resources that orally administered bizphosphonates are usually OK for minor oral surgery, with precautions and proper informed consent. The complications are reported mostly from iv administered bizphosphonates, and BRONJ being the most severe and debilitating. I understand that you have mentioned maxillary posterior region deliberately as it has good perfusion, and soft trabecular bone, lot of osteoblasts/cytes.
Last month, I placed a crown on an implant I had placed about 4 months ago in the maxillary premolar area in a 67 y o lady who took a 4 week holiday from her ACTONEL[Risedronate Sodium] with her physician's consent, and started her meds back a month after her Stage I surgery. She did fine, and healed well and the crown is doing well too.
I have no experience with Methotrexate myself though I understand it is mostly given in advanced auto-immune diseases like Rheumatoid Arthritis (besides chemotherapy for cancers) to suppress the body's immune response. It can seriously affect healing in dense bone. A few months ago, we saw a bad case of infection in a lower wisdom molar exo performed by a surgeon in Florida and the patient flew back here to Toronto, Canada after about a week. Soon, she had severe trismus, pus draining from socket, fever, pain,etc. Classic dry socket. Non-smoker and very careful type of person. I cleaned it out as best I could with her trismus, and had her on high Clinda+metronidazole orally for three days, but nothing worked. It quickly spread to sub-mandibular space and even her parotid space (scary) and then we had her admitted to a nearby ER where they put her on iv Clindamycin (Penicillin algy) and drained it from inside mouth for a day and then released her once she stabilized. This lady is about 51, a long term arthritis patient and was taking the new medication, called ACTEMRA for the last few months. I am not aware if the OMFS in Florida took any special precautions for this or not. I did detailed research but nowhere is it mentioned in their side-effects that dental surgeries to be avoided while on it. We even called their 1-800 number and reported this event. I am just their general dentist, but was able to chart the whole month-long ordeal as she finally got better. I would be very very careful doing bony surgeries in patients taking this category of drugs.
I hope the incidents I have described helps you to make an informed decision.
Good Luck!
CRS
7/23/2013
Just to clarify, what you seem to be describing is a post operative infection not a dry socket. Seven to ten days after surgery is the clinical time frame for that along with swelling and trismus. The treatment is iv antibiotics first not cleaning out or debridement which can spread the infection to the deeper fascial spaces which seems to have been what happened. The physician would take the patient off the medication prior to surgery since infections are a known sequela . I agree that I would not have removed a wisdom tooth in this case knowing that the patient would not be around for post op follow up and care. Also the infected sites need to be cultured prior to initiating antibiotic therapy in case the infection Is resistant to the selected antibiotic. Next time a patient presents with trismus and a fever I would recommend referral,the pterygomandibular space is contiguous with the posterior pharynx and can lead to airway compromise and much worse. I would say this patient was very very lucky. I also get an infectious disease consult in case things go south, this was an osteomyelitis waiting to happen. Thanks for posting, always ready to help.
KSD
8/23/2013
While I agree with your presumptive diagnosis of post-operative infection, I would have to say that your management is completely backwards. The treatment for an infection of this nature is incision and drainage first (cultures may be taken at this time) followed by empiric broad spectrum antibiotics. The antibiotic may be changed to reflect the sensitivities from cultures. Usually its mixed oral flora and doesn't grow out one specific bug. Never let the sun set on pus !
Hope this clears things up,
your friendly neighborhood OMFS
robert mann, dmd
7/24/2013
WHY? WHY EVEN CONSIDER THE PROPOSED PROCEDURE? AN IMPLANT IN THE MAXILLARY SECOND MOLAR AREA IN A COMPROMISED AND UNHEALTHY PATIENT. PROVE THAT THIS IS OF SUBSTANTIAL BENEFIT TO THE PATIENT. Measure the "risk vs. the reward".
RNM,DMD
Cliff Leachman
7/25/2013
I thought it was a typo, maybe he means multiples, I hope?
Can't be a single 2nd max molar in an otherwise dentate individual.
rsdds
7/24/2013
i 've had 3 cases of bronj in my office 2 with fosamax and 1 with prolia and my question is How bad does this pt want an implant in an upper 2nd molar?? is it worth the risk ??
Gary omfs
7/25/2013
I've had troubles both with osseointegration and early bone loss in the few patiënts on MTX that I did. I don't do them anymore. Combine this with fosamax and your bone has no healing capacity at all!
Peter Fairbairn
7/25/2013
The current issue of JOMI has its main Themtic review on this topic which is a very worthwhile read .
I agree WHY bother with a second molar case when there could be issues .
Having said that current research ( Jomi November ) show that Bisphosphonates can improve oseo-integration and just how small the risk of BRONJ in fact are .
Having worked and placed on many patients with full AIDS in the early 90s we have been suprised by the long term results in these immuno-compromised patients .
But in our letigious world is worth it , especially for a 2 nd molar .
Peter
CRS
7/25/2013
Peter Again wise advice, I will check out the article. I have noticed clinically that the litlle old ladies I extract teeth on Bisphos have very hard bone, and yes the risk is low overall. It is just such a litigious target, I have to give a deposition on this and I did not treat the patient only referred her to the appropriate facility!