Periapical Radiolucent Lesion: When is it Safe to Place Implant?
Dr. FB asks:
I have treatment planned an implant to replace #9 [maxillary left central incisor; 21]. #9 fractured and was non-restorable and I extracted it. It had a radiolucent lesion at the apex that was 6mm in diameter. My protocol is to wait 8 weeks after extraction before placing an implant when there are no pathoses. In this case I am concerned that there should be significant resolution of the pathosis before I place the implant. I do not know how long it will take for the infection to resolve. In a case like this, at what point is it safe to place the implant?
4 Comments on Periapical Radiolucent Lesion: When is it Safe to Place Implant?
New comments are currently closed for this post.
Carlos Boudet, DDS
8/16/2010
Dr FB
I assume that after you extracted the tooth you curetted the periapical lesion completely.
You also fail to say if you grafted the socket, which would reduce the amount of bone loss after the extraction.
Many surgeons are hesitant to graft the socket if there is a periapical lesion present, but using the Waterlase laser you can clean and detoxify the periapical lesion and prepare a bleeding socket for grafting without fear of infection of the graft material.
Due to the size of the central root and the size of the lesion, I would wait four to five months before implant placement.
Then depending on the amount of labial bone (2mm optimum), place a 4-4.3 implant of adequate length .
Hope this helps.
Carlos Boudet, DDS
Dr. Danesh from Iran
8/22/2010
Dear Dr.FB
Actually the only absolute contra indication to place the implant is acute infection.
But since you are placing the implant in esthetic zone you can have the socket preserved in order to make it more predictable,esthetically.
A good apical curetage is mandatory,to have the bleeding , disinfecting the area , and preserving the socket by using bio oss or hatcp ,and a Cobi Lansberg technique to seal the socket, and to place an implant after 4 months to be sure .
For the meantime just replace the missing tooth with an FRC to make it such a way to form a nice papilla...
Good luck.
Howie Gluckman
8/25/2010
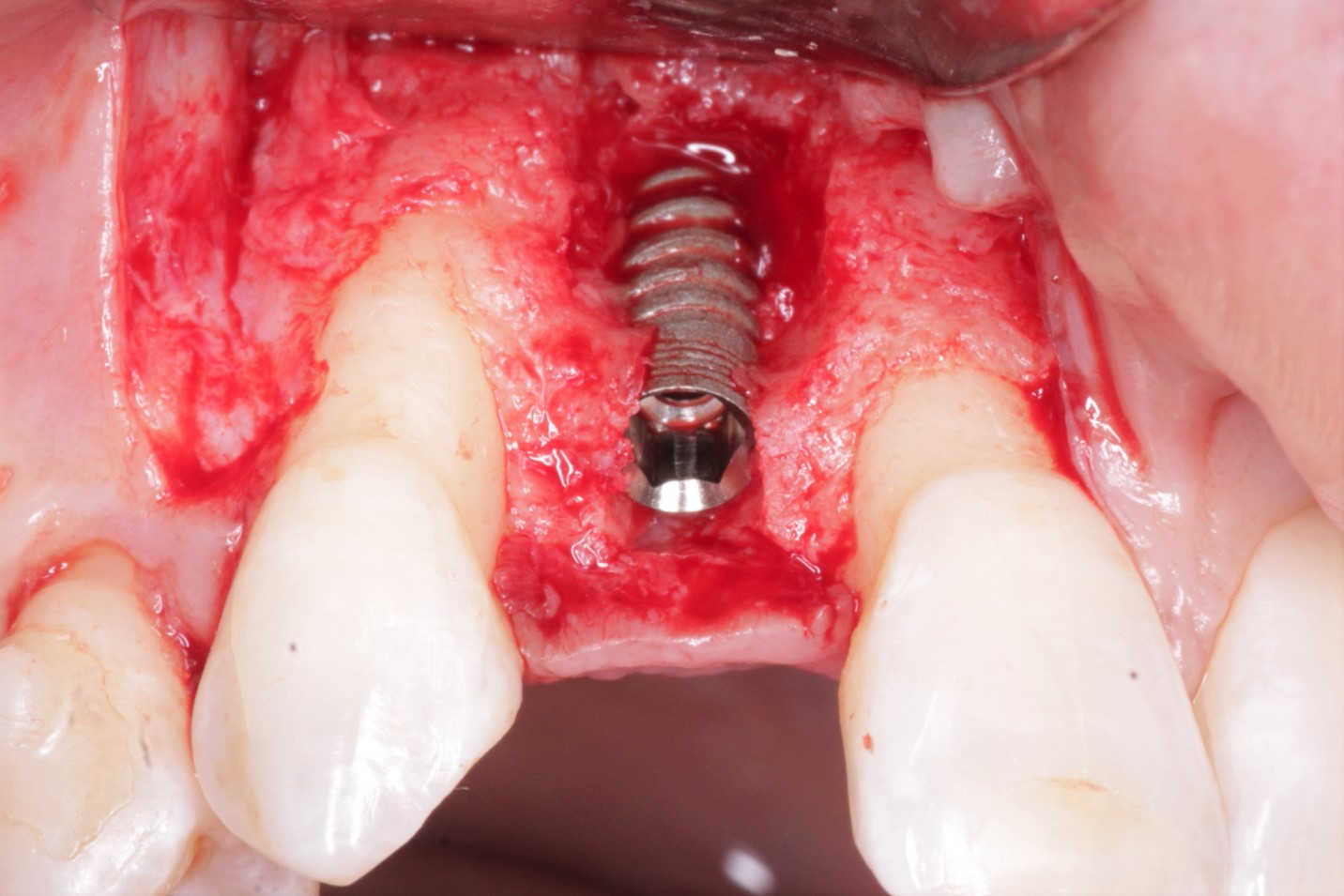
I have no problems placing the implant immediately into an area even of acute infection. the provisio though is that you can clearly see that you have removed all the active infection from the socket. It is essential to have good magnification as well as light source to be able to do this. I prefer not to do socket presevation as it prolongs the treatment for the patient and requires many months of healing before the socket is ready for an implant placement as it takes a long time for bone to form in the sockets. Just a personal preference. There is Data available to substantiate the immediate placement into areas of apical pathology and I will gladly give them to you if you would like them. I have also just completed an immediate molar placement study where no patients with apical pathology were excluded. It was a 3 year follow up study with 150 patients. we had 3 failures which gave us a 98% success. there are many other studies available. the ridge preservation techniques are all possible but it depends on how many procedures you want to put your patients through but everything works
ghariani
8/25/2010
I agree with Gluckman approach.we all know that inflamation participe in healing and it is more acurate to operate in the same time.if we wait for complete healing and re open the site we take the risk of making weacker the site