Post-op Pain after Resorbable Collagen Membrane use in Extraction?
I did an extraction of an endodontically treated tooth. I only used a collagen membrane and closed with sutures. Patient rinsed his mouth and looks like he lost his sutures the same day. It’s been 2 days now and he is having lots of pain. I suspected a dry socket, but when we looked, some of the membrane was already was gone and some epithelialization was seen. We went ahead and irrigated the socket. I exposed the socket and it was curetted and we achieved hemostasis. Patient was prescribed antibiotics and pain medications. Patient is still having pain but no swelling. What can be done now?
10 Comments on Post-op Pain after Resorbable Collagen Membrane use in Extraction?
New comments are currently closed for this post.
Dr. Gerald Rudick
4/25/2019
Give it some time......the patient has medication and will be feeling better shortly....are you sure that you removed the entire tooth?
Sean Rayment
4/25/2019
I had an issue once with ridge preservation of an extraction site that was treated with allograft and resorbable collagen membrane. The patient described similar pain to a "dry socket" but the graft was stable however the membrane was not secure and I believe the discomfort was from the membrane irritating the tissue. I removed the membrane and resutured but it took time for this to resolve. Sounds like you did the right thing, but next time an extra suture?
PerioProsth
4/25/2019
Not enough information. The most important factor is the tooth number. How can you forget to mention it?
if it is a dry socket, it has not been proved that Antibiotics will help, since it is not an infection.
Also, if it is a dry socket, it usually has a typical look, meaning an empty socket with little black blood clot and wherever you touch, it is sore.
Dry Socket paste is more appropriate to place inside the socket, in this case.
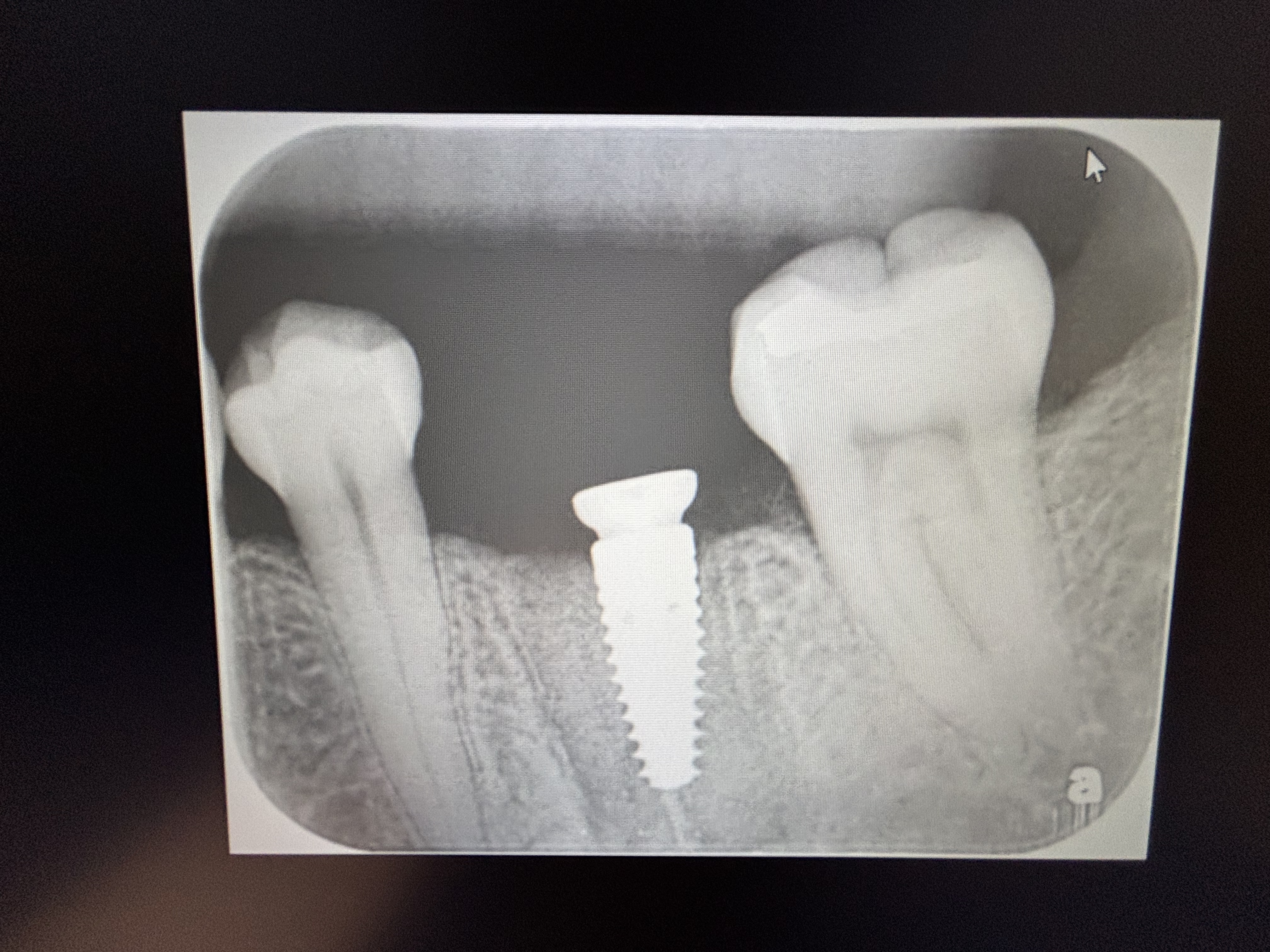
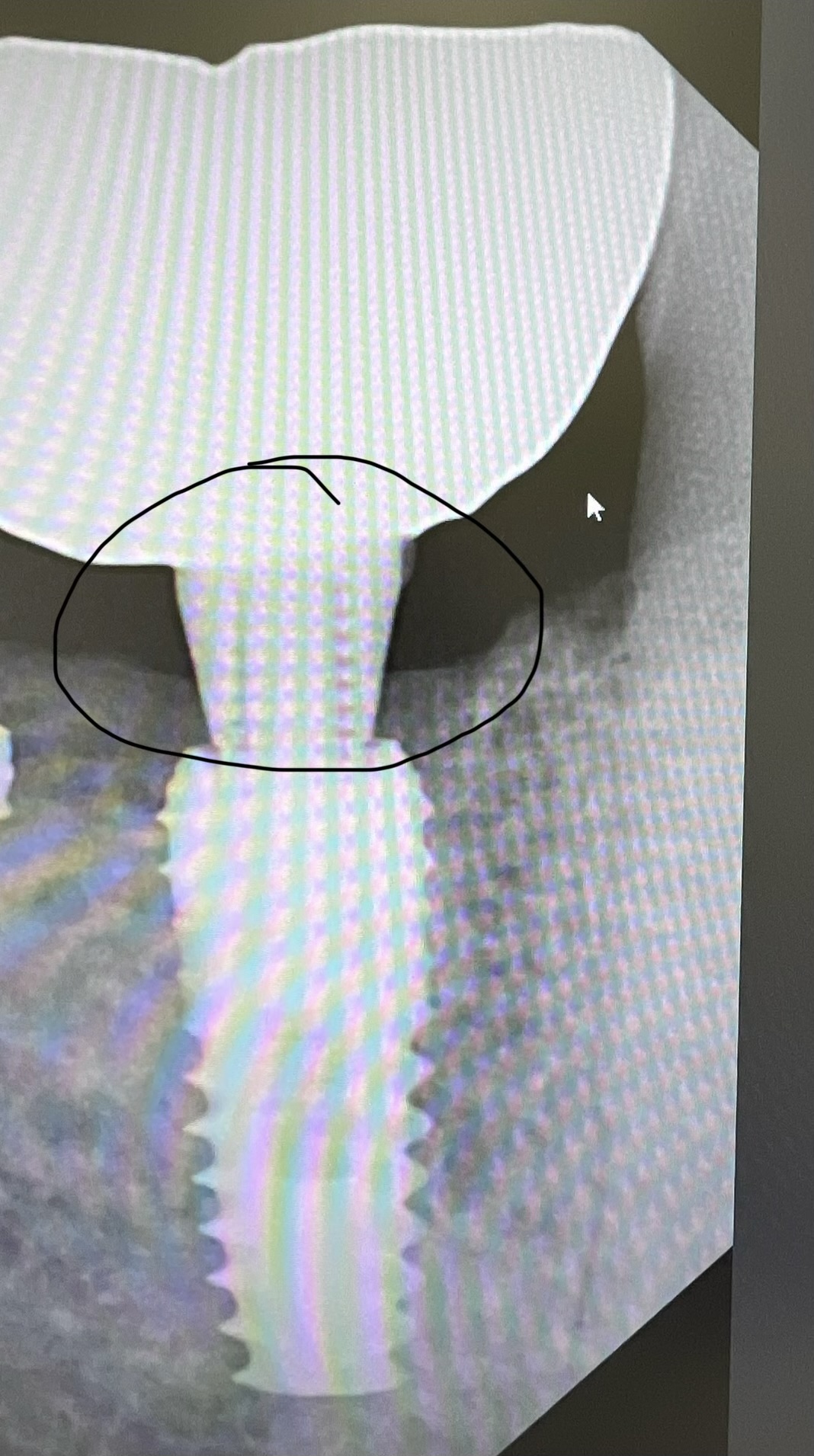
please provide before and after ext. Xrays and a clinical Photo of the socket from the Occlusal view if you have a camera in your office.
Rodgeru
4/25/2019
I have seen much more post-op swelling and pain using cross-linked resorbable collagen compared to non cross-linked. I have been using Biogide with better results, and the higher material cost is offset by fewer procedures and visits managing subsequent problems.
https://www.ncbi.nlm.nih.gov/pubmed/28617950
Dr U
4/25/2019
Treat like a dry socket
Sumit goel
4/25/2019
Nothing u shd do now . just wait n watch. Pain will be minimize with passing day... Only u could have used some alveogel kind of haemostaic agent to stabilize clot and cover exposed bone ...
Aly mahmoud
4/25/2019
I think pain is due to residual infection, socket preservation is an occlousive procedure
DreamDDS
4/26/2019
Yes it would be good to know the site . My experience as to this condition:
1. I am thinking this is a bicuspid probably upper; I say this because you used a resorbable membrane. A molar socket graft will seldom work with resorbable due to size of socket and patient over rinsing or sucking out the membrane. That is , unless you did a flap release and periosteal score to gain primary closure., in which case you would not have this issue. A PTFE membrane is needed; lift periosteum under from papilla to papilla to secure the membrane. Then X suture to secure.
This membrane will stay in place.
2. Post op pain in lower molars not unusual even if graft in place. Second molar pain more common . Was there a lesion and how many years for RCT. You need to aggressively debride socket and lesion. Long standing lesions , I find, have virulent and aggressive bacteria, need anerobe antibiotic like clindamycin pre -op in all cases; with suppurations add amoxicillin
If true dry socket then epithelium grows 1-3mm a day and pain goes away 1-2 weeks
Watch wound site. Does it look normal over time learn what healing stages look like
Good you did not go for immediate implant placement. I always approach extraction as difficult and 99% flap out to see the surgery field. Charge accordingly and you will cover these hiccups
Good luck
Dralfdel
4/26/2019
Not a lot of info on why the endo tooth was extracted. I had a similar case where the endo tooth could not be touched because of extreme pain. It got worse after extraction! Turned out to be trigeminal neuralgia.
Dr Dan
4/30/2019
I had a similar episode recently. Extracted #18, grafted, sutured. Pain started the next day, similar to dry socket. Dry socket pasted helped but needed to be applied 3-4x per day. After a week the graft was removed (TCP) and the problem was solved almost immediately.