Suture Lost Exposing the Implant: What to Do?
Dr. R. asks:
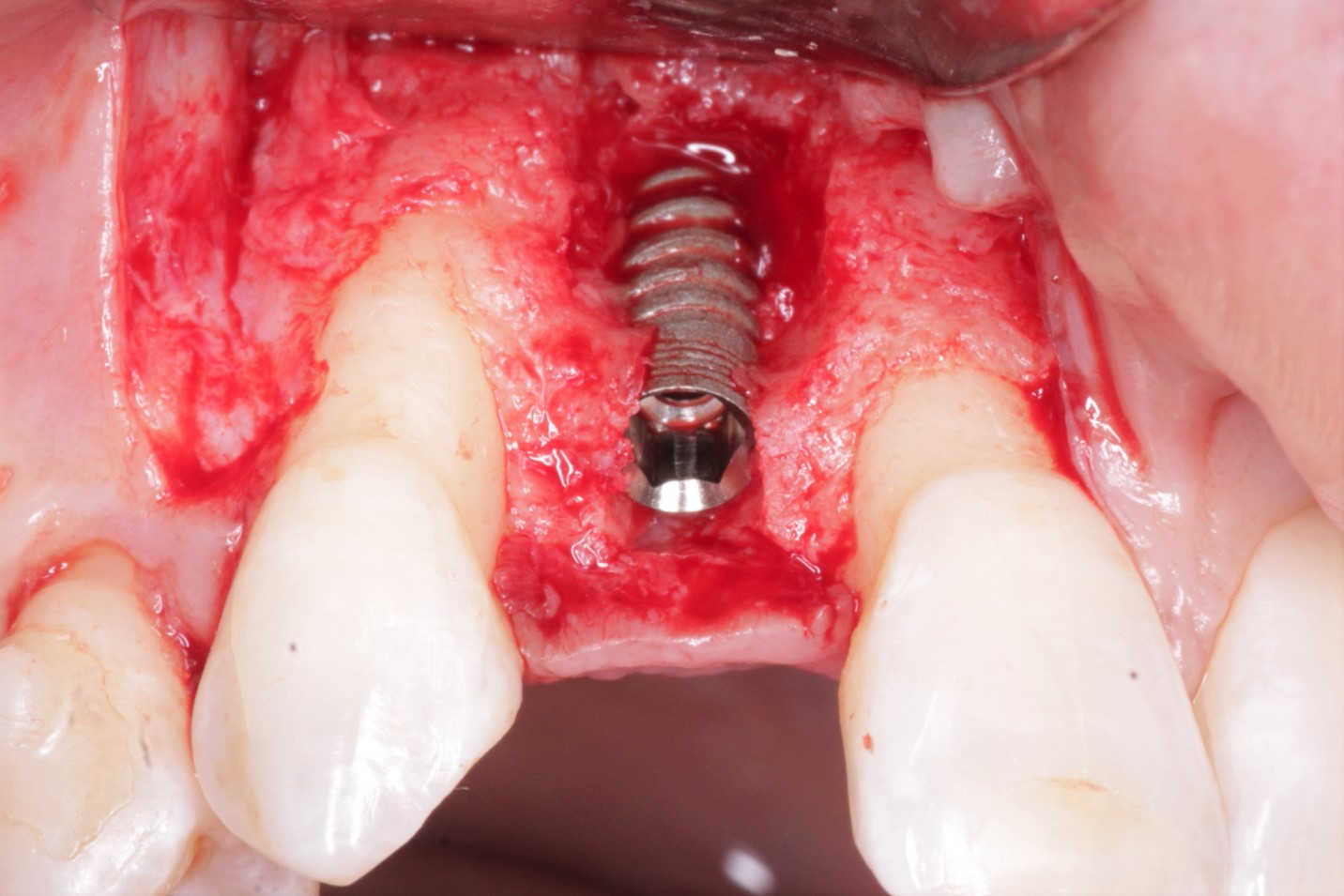
I extracted the upper left first premolar [#12] about one month ago and then after 2 weeks post-op, I placed a dental implant in the extraction site. I raised a full thickness flap but had some trouble with the sutures because the flap was thin and weak. After 3 days the suture was lost exposing the implant. I decided to leave the situation as is until the healing progressed to decide what to do next. I put the patient on Augmentin 600mg tid for 1 week and then clindamycin for 5 days and chorhexidine gluconate .2 % mouthwash. The patient still has some throbbing pain in the area upon palpation and the implant is still exposed. What should I do next?
62 Comments on Suture Lost Exposing the Implant: What to Do?
New comments are currently closed for this post.
Girish Bharadwaj
6/10/2008
If you are happy with the position of the implant it may be worthwhile debriding the area and cover the implant with a biogide membrane or the likes of it. This will help early mucosalisation and also acts as a barrier for ingress of bacteria.Hope this helps
Best wishes
elievictor
6/10/2008
Exposed implants are not a common post op complications, but always predictable. In those cases resuturing is required to close the wound , isolate the bone , to avoid more exposure and prevent further perimplantitis infection.
Chlorhex mouth wash + NSAID are enough. Antibiotic is not necessary.
Hope it helps
MainOralSurgeryman
6/10/2008
First Off Why are you prescribing antibiotics??????????????It guys like you that are causing all Clostridium difficile infections which there has been a huge increase as of late.
Next why are you entering into an extraction socket to place the implant 2 weeks after the extraction? Most of the research shows wait at least 6-8 weeks.
Next, even if you did need antibiotics, which you dont, why are you using such big guns. Then you are completely using them in the wrong fashion. You never just switch antibiotics just for the sake of switching. whats your rational for switching????????
Next to elievictor, if you understood sound surgical principles you should no you never close a dehisced wound.
My God I cant believe Im reading such thing like this.
This above case proves that you cant take a weekend course and be proficient at surgical procedures. Same day soon patients are going to realize there mistreatment and then god help us all.
Bruce G Knecht
6/10/2008
Hey, Oral surgeryman. This is a helping blog and not a crucifiction blog. Lets help each other with constructive hints. Thanks.
SFOMS
6/10/2008
To Dr. R,
I would not have approach this clinical case the way you did. In fact, I would either placed an immediate implant with a provisional temporary out of occlusion, or waited several months for osseous regeneration of the socket and to gain full epithelialization of the socket.
In either case, it depends whether or not you have primary stability. Did you really need to raise a flap where the blood supply was compromise from healing to begin with? Could it have been done thru the extraction socket? Also, where is the exposure? At the abutment platform or the threads of the implant wall? Exposed threads are not likely to gain bone growth, unless you have at least tried GTR.
mark hong
6/10/2008
Wow, chill out leave the newbie alone. I think we need to be in an environment of encouraging not chastising. I think even you osman would agree someone has to be your first case weather you are an experience oral surgeon or a dental student, we have to start somewhere. Let's encourage and teach the right protocol if you don't agree with what was done. Immediate placement is routinely done in the extraction site and many times implant head will become exposed. There are even protocol for doing non flap procedure which by definition will expose the head of the implant. If the patient cannot handle the normal flora of bacteria in the mouth then there are more serious issues than the implant. Do do more keep learning and you won't miss a step
Dr. Ben Eby
6/10/2008
When you have a dehisience, I see a lot of recomendations for Clorhexidine. My experience has been that Clorhexidine and other chemicals tend to kill bacteria and the new cells trying to grow over the area. I prefer saline rinses, and not to agressive, at that. The antibiotics aren't a big help, we don't often have infection. I prefer to place the implant at the time of extraction or wait at least 5-6 weeks for soft tissue healing.
Implant Doc
6/10/2008
I am sorry, but I have to agree with Oral Surgery Man. This is downright ridiculous. If this is how you to treat a VERY BASIC single unit case, you are a prime target for a lawsuit. Which weekend course did you attend?
Here is a little bit of advice...refer to someone that knows what they are doing.
Rand
6/10/2008
The two docs who are so hyper critical should not be so quick to be judgemental. This blog is dedicated to help. The doctor with the question has asked for help not criticism. No matter how experienced you are there are others with with more experience who could if so inclined criticize your failures. What goes around, comes around.
Several good suggestions have been made. In the end if failure ensues you may have to remove the implant, let the site heal and replace it after sufficient healing time. Removing an implant is simple to do. Under local, you just unscrew it. Currett out the granulation tissue, get the bone to bleed , place graft and get a good blood clot with our without a barrier.
Best of luck to you. And remember, every leading lecturer I have ever heard has always said that they learn more from their failures than from their successes.
PerthDentist
6/10/2008
Theory must preceed Application. These questions asked by Dr R display a fundamental ignorance of the theory of implantology, healing and all the possible modalities of dealing with altered healing.
I suggest all beginners start with courses/book/tuition before leaping into the mucosal gully strapped to a heavy expensive titanium anvil.
DrAshish
6/10/2008
Hi,
Keep the area clean with regular Chlorehexidine Mouthwash.If 'Exposed' means only coverscrew is exposed don't worry ;its just like having placed a gingiva former.
Email:info@drashish.com
Web:www.drashish.com
JP
6/11/2008
It depends.
If there was no bone augmenation, place a gingivaformer and a good suture. If there was bone augmentation, make a flap, curretage (bleeding !), Bio-Oss and membrane, healing screw and a good suture, let it integrate 6 weeks (2-phases).
Never implant 2 weeks after extraction, wait 6 weeks (soft tissue healing), or implant instantly.
Succes !
JP
Dr Naji Abboud
6/11/2008
hey guys, I don't want to interfere between implant specialists and weekend course implant doctors but of course some basics in oral surgery and tissue healing must be known here. Soft tissue healing takes between 6 to 8 weeks and hard tissue healing takes a minimum of 3 months after extraction. So as we see in this case the doctor wanted to place the implant in a 2 stage procedure and cover completely the implant, he had to wait for a minimum of 6 weeks.
The other way would be either placing the implant immediately after extraction or after some weeks in a single stage procedure and keep it uncovered that means with a healing abutment or with a temporary unloaded temporary crown.
Periodontist-beirut-Lebanon
John Clark
6/11/2008
I used to regularly prescribe post surgical CHX rinses but no longer do so after reading that CHX can have inhibiting effects of fibroblasts. I do however, still use a single pre-procedural CHX rinse immediately before surgery. My new norm for after placement care is salt water rinsing 3 x daily for a week commencing the following day. To date, all has been well. Also, if you were going to GBR over the defect, it may be prudent to cleanse the exposed threads with a citric acid wash as recommended by Carl Misch.
Don Callan
6/11/2008
Do not use Chlorehexidine Mouthwash after surgery--John Clark is correct, it will delay the healing process. However, what is the deal with citric acid--where is the literature support for the treatment with citric acid?
MainOralSurgeryman
6/11/2008
To all those who say im to harsh and that this site is dedicated to helping not bashing.
I feel I am helping......Im helping the patient and helping this Doctor avoid a lawsuit.
When did we forget what it means to elevate the profession to a high level. Part of the problem in todays profession is we except mediocrity or minimal acceptable treatment as a passing grade.
Ask yourselfs "DOCTORS" would you accept the above if it was done on your Loved one????? I dont think you would. The same guys that are screaming at me that we need to help would have a fit if this was done to someone in there family.
Doctors we are working on PEOPLE we arent working on Maniqiun heads.
Minimal acceptable treatment is becoming the backbone of dentistry today. WHY? Kids today are coming out of dental schools with few clinical skills. Ask some of you friends that work at GPR's or AEGD's they see young dentists who did 2 crowns in dental school or 5 canals of root canal. Yet these same people want to rush to do sinus lifts, block grafts, implants and advanced surgical procedures in which they dont have the basic dental knowledge yet alone the surgical knowledge to do the care that patient need.
I love this statement "And remember, every leading lecturer I have ever heard has always said that they learn more from their failures than from their successes." Those same lecturer will tell you that there practices are overflowing cleaning up messes of surgeries that people should not have been doing. Just ask Pikos or Froum off line. I even have seen Froum speak recently about implant complications and he spoke about case after case about patients that have come to him with implants floating in the sinus or nerve damage which he joke about contact you malpractice before you start.
What do you think the patients do after the leading lecturer to cleans up the above implant mess???????? They contact thier attorny. Who do you think is going to pay for all the work the the leading lecturers have to clean up.
There is a case in my home state that a Dentist is losing his dental practice because of a implants he missplaced in the sinus and ultimately perforated the orbit of the eye.
When did we become a profession when we forgot to refer. Is it all about the Money?????? Have we forgotten about actually caring about the patient. Dont get me wrong am not one of these oral surgeons that feels all surgery should be done by surgeons. I have plenty of general dentist friends who do good surgery and implants, yet they know there limitations and refer when needed. There is a problem with our profession when periodontists and other specialists are going out of business. Have we cured periodontal disease?????? I dont think we have. WE forgot that dentistry is about health care and made it more into a business.
LADIES AND GENTLEMAN we need to police our profession and we need to elevate our profession to the next level. We cant expect minimal acceptable treatment and above all we need to remember we are working on people. Working on a patients as we do is a gift and shouldnt be taken for granted.
Either we elevate our profession for our patients sakes or the Government will elevate it for us.
Harris
6/11/2008
I happen to agree with MainOralSurgery man.
A "surgeon" is not a "surgeon" because of the 99 that go easily, a "surgeon" is a "surgeon" because they can handle the one that goes badly.
With that said, none of us has enough information about that case to be judgemental!
I see this a lot, Doctors bashing Doctors because they assume they know the whole situation. Which is rarely the case.
The above post could be a major problem or a simple minor exposure.... we should offer guidance without judgement... if for no other reason than we don't have the whole picture sitting in our OR.
JAV
6/11/2008
The most important thing we need to learn from this case is case selection. Implant companies will sell these products to anyone at anytime. The most important fact we can get from this case is that placing the implant after two weeks did not allow the bone or soft tissue any time for healing.
If this is one of your first cases, you need to select a simple site with good bone and good tissue. Thin tissue is a problem that should have been noted prior to surgery. You need to have the basic knowledge of any surgical procedure prior to starting. Primary closure is difficult in any extraction site.
The problem here is not that the implant is exposed, but where the exposure is. If the pain is on the facial and the bone loss is on the facial, this will be an esthetic problem. The best treatment would be to remove the implant and graft the socket. Let the area heal then go back in and place the implant.
Once you laid the buccal flap you disturbed the blood supply to the thin buccal plate of bone. In the area of the first bicuspid I would not try to just watch it. With thin tissue, this is a difficult area to graft. Good luck with this case.
Harold Bergman
6/11/2008
Why did you raise a flap for an extraction site implant placement? Do you flap over every extraction site? Place the top of the implant 2mm below the crest of the bone and the site will heal just like every other extraction you have done. KISS
Dr S
6/11/2008
Main OS MAN
How about a clinical oppinion that is relevant to this forum?
Or shall we make this a discussion about the ivory towers and poitics of dentistry in north America ?
This is a world wide forum and not every body is as great as you ..this is not life threatening and the implant may be lost ..and another one placed ..and it will be a service to the paetient and the Dr will be more experienced.
Your last post could have described the entire procedure in detail (which would be very helpful to many I am sure)instead we just have angry rhetoric .
Nobody reads the forum for that
MainOralSurgeryman
6/11/2008
Dr. S your attitude sums up the problem with treatment of patients today.....Your attitude of no big deal the implant will be lost but just place another one.
HMMMMM anyone have a problem with that.
Any thought of what the patient has to go through to get another implant??????? Cost, time, pain,......just add to the list.
Never mind the fact that if the patient does loss the implant you probably now have relegated patient to get a big bone graft to regenerate the bone that was lost due to the Doctor not knowing what he was doing in the first place.
O and where did I say I was better then anyone else. The point is Dentists should know thier limitations and think about the patient needs and not just there pocket books.
Last I checked this is a blog site. Not everyone looks at things through rosey glasses, you may or may not like my opinion but its reality no matter what country your from.
In your opinion has there anything that I said "IN MY FIRST POST IN THIS THREAD that wrong???? If you think otherwise you obviously dont read any articles or understand what evidence based dentisty is about.
Anybody can do an implant, but understanding the basic surgical concepts is another thing. Most of that info can be found in any journal if you just take the time to read and learn.
osurg
6/11/2008
Dear J.P.
You make an interesting statement that one should never place an implant two weeks after extraction. Would you please support this with evidence based research. The reason I would like to read that is that I have placed a least 50 or so implants shortly after extraction and had no failures. This is not how I prefer to operate, however often patients have not made up their mind and need immediate extraction to deal with an emergent problem. As I stated placing the implant one or two weeks later when they have decided has caused no problems. Actually, it has avoided having the patient feel that they are pressured. Perhaps we could elevate the level of this cite if we avoid catagorical statements without evidence. I Find that in medical and dental schools too many statements are accepted as fact and perpetuated because someone said so. I might suggest we all read an excellent book "How doctors think" we all would be better at what we do.
John Clark
6/12/2008
For Don Callan (and anyone else interested)
Don, Misch recommends detoxification of the implant surface with 40% citric acid, pH 1 applied with a cotton pledget or camel's hair brush for 30 seconds. This protocol arose from a study by Zablotsky et al: The ability of variuos chemotherapeutic agebts to detoxify thye endotoxib infected HA - coated implant surface, Int J Oral Implant 8:45-50, 1991a. All this and more in Misch's Contemporary Implant Dentistry 2nd Edition pages 651 - 653.
John
Dr S
6/12/2008
Mr Angry mainoralsurgeryman
Any chance of a clinical and relevant opinion?
MainOralSurgeryman
6/12/2008
Dr.S....That was a Great response.
I believe all the clinical points were in my first post of this thread. Why dont you enlighten us on how you would handle the clinical situation from above. Please feel free to back up your treatment plan of the above patient with sound research.
O wait never mind, you already comment on how you would just slam another implant in there.
The only guy who is angry around here is you since you obviously cant handle the reality of what I am saying.
Roy Mintzer
6/12/2008
To all: Believing that lighting a candle is preferable to cursing the darkness, I think that it benefits all to remember that specialists differ from generalists by 2 major points: They/We have additional years, not weekends, of training and limit our practices to these types of procedures. If you interests take you to a comparable level you should do implants, grafts, etc. as a GP. I believe that being accomplished in implants takes the same amount of time as mastering endodontics. Can you make the commitment? If so, go for it, if not, refer.
As to clinical techniques, I find that initial use of a ProphyJet to "sandblast" the implant works well. Citric Acid or Tetracycline has to be applied with cotton and I'm always worried about leaving fragments behind, even with magnification. Also, placement of an implant 2 weeks after extraction is such an obvious mistake (to a surgeon) that you'll be hard pressed to find a study that tests this specifically. If, on the other hand you read the literature about other methodologies they invariably wait a longer period - basically place it at extraction or wait. Thanks
osurg
6/12/2008
Roy please elucidate why you can't place an implant two weeks after extraction. Why is it so so "obvious", I am a surgeon with over thirty years experience, placing implants of all types for over twenty five of those years. I previously stated that I have over 50 cases of slightly delayed placement and they all worked without complications. I do not advise that this be the standard mode of treatment ,however, I do not accept your absolute prohibition. By the way, "obvious" is a somewhat snide comment.I thought we were going to try to avoid this. Think back when we were told implants had to be covered when placed or they would fail or we must wait six months to load. What was "obvious " does not seem to be immutable.
MainOralSurgeryman
6/12/2008
OSurg while I appreciate your commments about the whole concept of 2stage vs 1 stage implants back in the day. A mentor of mine way back told me that surgical concepts should be based on what makes physiologic sense within the concept of wound healing.
Just because your approach has worked in your hands doesnt mean that the time tested concepts of wound healing should be ignored. I would even argue the fact that because you have 50 success under your belt that you have probably gotten lucky 50 time. Although there is an old saying I rather be lucky then good. I therefore wouldnt reccomend that you advocate telling Dentists in this forum that its ok to place implants after 2 weeks of healing just because you have 50 successful cases in your office. If you want to create a new protocol I suggest you publish your data in a peer reviewed journal.
With that being said I would recommend that if you going to place implants in a delayed approach you wait at least 6-8 weeks ( with some articles saying 12 weeks) if value the concepts of wound healing.
Here are two articles to support why taking into account human wound healing, one should wait at least 6-8 weeks before placing an implant in an extraction socket and there are ton of other articles.
Soehren S., Van Swol R.: The healing extraction site: A donor area for periodontal grafting material. J Periodont 50:128-133, 1979.
Evian C., Rosenberg E., Coslet J., Corn H.: The osteogenic activity of bone removed from healing extraction sockets in humans. J Periodont 53:81-85, 1982.
Roy Mintzer
6/12/2008
Osurg, you're right, my use of "obvious" was flip, if not snide. What I meant was that if the implant can not be immediately placed there physiologically won't be any more bone 14 days later. Wound healing requires a cascade of events, with mineralization being the last step. If our implant isn't stable at time of extraction we're not going to have vastly different environment 2 weeks out, save for a more granulated tissue at the coronal aspect. If that's what you're looking for, then grafting/barrier membrane should give you that at the extraction and you can do the immediate.
Ron Neff
6/12/2008
Dr R-
I am projecting that you are relatively new to implantology. Forgive me if I am wrong. It is difficult to know the exact circumstances from your question so I am risking making some assumptions. My intention is to shine some light on the issue... Hope this helps.
Start with these items:
First, communicate with the patient. Decision Tree, Prognosis at each stage, maybe a percentage estimate, additional costs if any.
The malpractice issue yields best to a patient who is not in the dark or in fear. So something like: We will clean up threads and cover them with a graft, it is about 50-50 (under promise, over perform), if it 'refuses to heal' we will remove the implant, graft the socket and allow for healing [(be conservative now) 4 month min for the lower, eight months for the upper---others may recommend differently---(this is intentional erring on the side of prudence after a misadventure in the outset, and now assumed in the attempted repair)], only then replace the implant; finally you may want to allude to referring to a specialist as the last step in the decision tree. I am not saying to generally refer last, and in this case you are already committed... So it maybe a good call here.
Then evaluate the reasons for the failure. Operator error is being shouted at you shrill-ly. Okay, if that is it; accept it, and grow; what else, cigarettes, (closet pot smoking!), excessive or compulsive rinsing, brushing, poking, tongue-ing the area post-operatively, diabetis, alcohol excess, medications, immunity, age tissue type... the whole nine. Note these things realistically. And it maybe both operator error and compromised healing together.
Continue learning, a lot of differing opinions are out there, take things with a grain of salt, pick easy cases to begin, lectures haven't in my experience emphasized their failures, they teach from their successes. We all have failures, or else well developed denial!
Handling less than stellar outcomes is an art in itself---when you acheive competance in this art you will be accomplished. It takes the challenges that come with a few exposed threads.
When you ask for help, do not be deterred by the loud-mouthed know-it-alls, or the sauve tongued seducers. Listen to all openly, even the boor, and the cheer leader, for they have insight amidst the cacophony, then do what works best in your hands. This is done by practice---it is called dental practice.
Here are some other considerations:
1) Osteogenesis transits high osteoclasis at ~3 weeks, sometimes called die-back. A bad time for integration.
1a) Either do a same day implant in the future or wait. I think suggestions about six weeks based on soft tissue healing undervalues the concept that it is the bone we are concerned with here. I'd wait longer.
2) Exposed threads can be difficult to cover so practice will be required... and proper patient communication.
3) All soft tissue must be removed from the surface of the threads, some recommend a laser for this---details would better be derived from a laser maven, not me.
4a) Citric acid seems to have some literature support, the surface definately needs to be treated with a cleansing agent.
4b) Not Chlorohexidine, see the film it leaves (brownness), logic suggests it is not going to leave a clean titanium surface (interface)for ossteo-integration. (The same from cigarette tars).
5) Cover the whole implant and graft with a membrane before closing it. Maybe a two stage non-resorbable (Gore-tex) would be best unless you are very experienced with membranes. Do not be lulled into a false security by membranes that can resorb before the job is done. They are often cheapest to buy.
6) Grafting is a whole 'nother chapter. Use allograft if you can. Puros, various cancellous or cortical donor bones of small particle size are good. I use demineralized mixture of the above with sterile Calcium Sulfate (plaster). I use a dash of clindamycin injectable as part of the liquid and sterile water or blood some times, too.
Bio-oss is a xeno graft (bovine), it may have a role here.
Some will say autograft is the "gold standard" If you are not familiar with the technique do not do it, put it on your continuing education list.
Make sure the entire implant surface is cover with graft, up to the cover screw occlusal. I say too much bone is a quality problem whenever I have to remove some over the cover screw or along its sides. Also, I rinse the implant cavity, and dry it and put a trace of formyl creasol on a dried applicator before the close the cover screw, no need having bacteria growing inside the work area.
If you have more questions about my pet techniques you can contact me 818-991-2757.
Also Garg's latest book is a good reference and easy read for a broad spectrum background text. Misch also has a good reference text. These are more complete than weekend coursework and more methodical than lectures from slides.
Good luck.
RNeff
eric wallace
6/12/2008
You are dealing with a wound dehiscence. Systemic antibiotics are not indicated. Chlohexdine rinse is okay, however it has been shown to cause inhibition and death of fibroblasts in early wound healing. I would dilute the peridex with saline. All you are really trying to do is stop plaque accumulation in the wound. Entering an extraction socket at two weeks is not a good idea, your tissue is weak and immature and it will not hold sutures well. What part of the implant is exposed. If threads are exposed do yourself and the patient a favor and remove it ASAP. If it's just the cover screw you will most likely be okay. I do not recomend any GBR, it sounds like your problem stems from a lack of basic surgical principals. Read some books, take some classes, and find a way to watch some specialists do cases. I have no problem with GP's doing surgery, as along as they do it well.
osurg
6/13/2008
Roy thanks for the responce. I did not explain what the situation was. The sites I placed the implants in were good sites. There was no shortage of bone. The only problem was that the patient had not decided on the course of treatment and was in pain. The extraction could not be delayed. I totally agree that if there is not enough bone on day one then there will not be a good site two weeks later. Sorry for not explaining this better.
osurg
6/13/2008
As an addition I should say, the site must be refreshed proir to placement with good bleeding assured. So in fact you have a situation that is like the day that the extraction was done.
RTKR
6/13/2008
Interesting thread going on here. I have something for American providers to consider. The US lawyers are beginning to solicit cases for dental implant malpractice. They have realized that this is an untouched gold mine for them. I have been called as an expert witness in a few cases. All cases were against general dentists that got in over their heads. The waters have been chummed and the sharks are now coming to feed.
Amr Bokhari
6/15/2008
I have posted a similar situation on Implant Cases under the title "Implant Dehiscence". A 55 y.o. female was referred from GP re: #30 implant bone loss. The implant was integrated 4 months postop. I reflected a flap, used tetracycline for 2 min., grafted with Bio-Oss and a Biomend membrane. A 6 months postop radiograph showed complete bone regeneration. I will include the postop PA radiograph shortly.
JW
6/16/2008
The citric acid thing was put forth initially by Cochran to detoxify exposed HA surfaced implants. The first step was to remove ALL exposed HA with a rotary instrument, so apples and oranges. There was also a more recent study that looked at TET, CHLX and saline, in vitro. All removed bacteria (TET and CHLX better)and it was the mechanical aspect that was important. The prophyjet thing works well, it's just really messy. In terms of Chlx post-surgically, the study most who worry about fibroblasts quote is from Jolkovsky, DL. Yes, it was found to be fibroblast toxic, but in a petri dish. The staining is thought to be an interaction between the CHLX and food, not a residue left behind from the use of the agent. Chlx was found to CLINICALLY enhance postsurgical results. Evidence based. J Periodontol. 1989 Oct ;60 (10):570-6
BTW: I don't think it is KISS if you stick the top of the platform 2mm sub-crestal. Seems a bit deep to me, but maybe I misunderstood.
anon
6/27/2008
"Interesting thread going on here. I have something for American providers to consider. The US lawyers are beginning to solicit cases for dental implant malpractice. They have realized that this is an untouched gold mine for them. I have been called as an expert witness in a few cases. All cases were against general dentists that got in over their heads. The waters have been chummed and the sharks are now coming to feed."
Are you sure about that? I have a legitimate case and I can't get any lawyers to bite. With signed consents they feel patients get what they deserve. Maybe you are interested in pushing out competition. Consideration needs to be made for the fact that heavily invested implant reps are teaching quick start courses and giving false confidence. A push for regulation like any other industry needs to be made.
TRACY
6/30/2008
I came across this site while researching info for further implant treatments i would like to have once my current implant has been completed. I have already had my first post put in and i am now waiting to have the actual "tooth" attached. So far so good. I am one of the "nervous" patients you must dread having!!!!!! Now i would like to say how i greatly appreciate the patience of my own dentist and the confidence she has given me in being able to even contemplate implant work. Im sure this patience also applies to many of you learned dentists participating on this blog. HOWEVER, i would also just like to point out that although i agree with the point that "every one has to start somwhere" please please please have in the forefront of your mind that this is a HUGH deal to many of your patients both mentally and more importantly phyisically if the consequences of your work are not done with complete knowledge backing up your scalpel! The impression one is given here is that somewhere one of us "civilions" is going to become one of your "guineapigs". Finally after going thru childbirth 3 times and going thru a botched dental treatment (with a ex dentist!) i can whole heartedly say there is no hell on earth like a dental pain and have spoken with many many people who say the same. Frankly it has got me rather rattled to think i could have been the patient of someone who has been on a weekend course and potentially left me in agony.
TRACY
6/30/2008
P.S, mainoralsurgeryman, I salute you!
ACabero
7/3/2008
Dear Dr. R,
I would like to ask first if there are granulation tissues forming on the wound already. If so, you have to first anesthetize the area, then clean the wound thoroughly with a currette without damaging the implant body. Just remove the soft tissues so that the healing will be more promising. Then debride the wound with citric acid to disinfect the area then with saline solution. After which, you prepare your resorbable membrane. Then suture. For post op, you just prescribe NSAID. Then ask the patient to rinse with saline solution as often as needed. The reason for the pain is that since you have left the wound open, it is readily attacked by opportunistic microorganisms thriving on that area. You are only inviting more bacteria to thrive on your implant site, which should not be the case. Just keep in mind that when sutures are removed prior to the required 10 days of healing period, you can always suture the wound back. Clean it first then re suture. In this way, you can save yourself the trouble of thinking if the implant is successful or not.
peter Shieh
7/3/2008
most of us fell a couple of times before we learned to walk. It is now 6 weeks after placement.with a explorer check for mobolity.If it is mobile that implant will most probably not integrate.If not mobile & if it can be restored let it be. Hydrogen peroxide is better than chlorhedine for rinces.But warn the patient not to rince for more than 10 sec. Good luck.
RTKR
7/3/2008
3 words...STANDARD OF CARE. That is what the savvy lawyers are using in these cases. If a weekend warrior Gen Den is placing implants, they are going to be held to the standard of care for said procedure. Lawyers are getting around the consent issue by showing that the Gen Den did not fully inform the patient of their dental implant training, expertise, and experience. In a court of law, blaming everything on the dental rep does not fly. Ultimately, everything is the responsibility of the provider.
“Interesting thread going on here. I have something for American providers to consider. The US lawyers are beginning to solicit cases for dental implant malpractice. They have realized that this is an untouched gold mine for them. I have been called as an expert witness in a few cases. All cases were against general dentists that got in over their heads. The waters have been chummed and the sharks are now coming to feed.â€
Are you sure about that? I have a legitimate case and I can’t get any lawyers to bite. With signed consents they feel patients get what they deserve. Maybe you are interested in pushing out competition. Consideration needs to be made for the fact that heavily invested implant reps are teaching quick start courses and giving false confidence. A push for regulation like any other industry needs to be made.
anon
7/3/2008
"3 words…STANDARD OF CARE. That is what the savvy lawyers are using in these cases. If a weekend warrior Gen Den is placing implants, they are going to be held to the standard of care for said procedure. Lawyers are getting around the consent issue by showing that the Gen Den did not fully inform the patient of their dental implant training, expertise, and experience. In a court of law, blaming everything on the dental rep does not fly. Ultimately, everything is the responsibility of the provider."
I have been told otherwise. Unregulated implies there are no standards. Anyone can teach or provide services. And damages are not awarded to situations that are considered reversible by simply removing the implants.
I also applaud mainoralsurgeryman. However, the Doctors asking questions at least have the integrity to confront their situations and are working to find help for their patients. And there are less fortunate patients that are left to find their own solutions.
R. Hughes
7/4/2008
We all started as beginners. Get more training, as much as you have time for. The AAID Maxi courses or the Misch are ageat places to start. Get credentials from the AAID. This helps alot. For the most part, if you are dedicated you can learn the material and techniques. R. Hughes, D.D.S., FAAID, FAAIP, Dipl. ABOI/ID
Dr SDJ
7/16/2008
To
MainOralSurgeryman
Sir, Since you comments were so presumptious and demeaning that sitting across the globe I feel hurt & I have been contemplating over weeks how to refute your high sounding but basically ridiculous premise about who should be doing implants & who should not. It was over two such incidents in one day that my views on the matter solidified.
You "ESTABLISHED" implantologists may have created a niche for yourself but don't give us the Bullshit about implants being so tough that no one can ever learn. I have been observing implants closely for last few years and find it to be as tough as say a root canal, and apexectomy, a wisdom tooth removal a long span bridge or a smile redesign.
For all the mumbo and jumbo that you guys create around Implants, so that you can fleece your patients, it's my observation that it's much easier and simpler than lots of other parts of dentistry, and mind you there is a lot to dentistry, from handling a bawling kid to stopping profuse arterial bleeding.
And about the ghost of failures let me remind you, you specialist guys correct our failure cases but there may be other specialists correcting your failure cases.
Well apparently the surgeon should be doing "appendectomies" and the physicians should treat "breathing disorders", but in dentistry every one is a surgeon whether a general dentist or a University degree holder in Specialized dentistry e.g. periodontist or OMF Surgery.
There would be General dentists who keep in touch with the latest and keep with their academics like "yours truly " does. And there are General dentists haven't visited the yellowing pages of their text books in decades what to speak of latest Journals and papers.
So you can't lump the "conscientious, sincere, knowledgeable" General Dentist along with the "out of touch and disoriented and ill informed†general Dentist. That would be, not just unfair, in my opinion, but also demonstrate openly to this forum, how much devoid of fine intellect you are and how your unjustified claims to High intellect and special training are.
And considering that we are across the globe, you presumably in the US of A and I in INDIA, that would be enough of an insult to you, may be out of proportion, to your sick comments.
Never disparage a colleague harshly. You were fortunate to get into a post graduate program and acquire a degree in specialized dental surgery, but you haven't the slightest of the proofs with you to prove that the humble general dentist is mentally retarded enough to deserve your tirade.
We family practitioners can explain to patients in simple language truth fully and honestly that which you specialists can't with fancy secretaries, marketing agents and fancy patient education software.
Today I received a call from a pedodontist to whom I referred a case. This wasn't the first time I received such a call. He was not interested in treating my patient. For blah’ blah reasons.
And also today I was talking to my favorite Oral Surgeon regarding difficulty with some implant cases and he started on the same track on which your good self went. He was telling me how my implant company was taking me for a ride and all the standard bullshit, all the specialist Implantologists, living in lofty towers, and driving Ferrarris love to tell.
They ask for references, and when you send them the patients, they act tough! So the specialists like to have it both ways they want patients and when you send patients they like to refuse making you wonder what went wrong.
So the analysis of the situation is simply that “If the patient is rich you send him to me and I will do the needful - If he is poor obviously I won't treat him even if he is willing to cough out the money and neither should you".
When we treat, the specialist assumes the worst, and when they treat then “failure rate of the procedure is high Mr Jones and I am sorry but the treatment failed to achieve our combined high objectives".
Sorry MainoralSurgeyman over the years I have developed a very low opinion about specialists and now you have gotten yourself added to my list of disgusting specialists. If there are any Ad-hominem attacks against you, which are barred here, I would be sorry to say that you deserved them.
And now a note for New Implantologists-don't let any one or any thing discourage you. Remember these guys are just protecting their bastion or territory from us mongrels. Most conscientious dentists are fully qualified in attempting Implants albeit after training even if it be a weekend one. (Some of these specialists often do crappy work themselves I have witnessed that often!)
Down with the bourgeois!
GA OMFS
7/29/2008
Augmentin, then Clindamycin... for wound dehiscence??? Forget the discussion about weekend courses for implants. What about basic pharmacology and microbiology? This haphazard prescribing of antibiotics, without clinical indication and evidence based practice is beyond excuse. These two antibiotics in particular should only be prescribed using established protocols for antibiotic prophylaxis (clindamycin, in pen allergic patient) or culture guided(Augmentin). Hope they aren't teaching this indiscriminate (and inappropriate)use of antibiotics at a weekend course. Have to agree with maineoralsurgeon on this one.
SerioPerio
8/5/2008
I have read this thread with great interest. There seems to be several points to clarify:
1. How much of the implant is exposed? An exposed cover screw is not a major problem. Gentle cleansing with a damp cotton swab with water usually keeps the cover screw clean. If the body (neck and threads) are exposed after such a short time, there is a major problem.
2. Implant surgery is generally close to painless for the patient. Continual throbbing in the surgical site is not normal and could be indicative of infection or a mobile implant.
3. All practitioners should remember the biology of bone (including the healing extraction socket- 8-12 weeks show high levels of bone activity- Evian- J Periodontol), soft tissue wound healing, pharmacology, anatomy, and any other aspects of our discipline. Thorough knowledge of the biologic principles will keep surgeons out of trouble.
4. Checking blog entries for spelling and grammar mistakes before posting will help promote excellence, both in surgical technique and commentary thereon.
SFOMS
8/5/2008
MainOSman, well spoken. But sadly to say, the messenger is sometimes prosecuted before the message gets across.
R. Hughes
8/6/2008
To mainoralsurgeryman: The field of dental/oral implantology was poineered and developed by GP'S. I have been mentored by these men. Tatum ( developer of the sinus lift), Roberts and Linkow. Linkow even developed the internal hex along with numerous othe developments. The OMS and perios are Johnny come lately to the field. You are welcome for the history lesson!
R. Hughes
8/6/2008
Dr. R, As long as you do not have the sides exposed and the implant is fixated and out of danger from any trauma from eating etc. You will be ok. Also have the patient clean the site with peroxide or periodex. This is usually no big deal. The pain is mostlikely from bone expansion (will go away soon), over heating of the bone-not good, or residual infection. One course of empiric antibiotic use is ok. If the threads are exposed then reflap with release, detox the implant with citric acid, graft with osteogen, suture tension frss, protect with an essex retainer.
Dr SDJ
8/26/2008
It seems all Oral Surgeons are ganging upon us lowly general practitioners for being stupid enough to attempt implants! Well if it weren't for us making those stupid mistakes who would refer cases to you Oral Surgeons? Your business runs on our fallibility! So just guide us if you can without making any nasty comments. We know you guys write text books and are "Brilliant". We see your 'spectacular' results day in day out. Yeah we see the cases you guys present on forums and what you guys really do in your practices. Your scraps with patients your exaggerations and unnecessary treatments. We notice everything, we may be diplomatic about it, but our eyes and ears are open.
Remember even we help you get out of trouble when you say stupid things to patients (like what you have written in black and white in this thread). We probably should stop bailing out your **sses next time around. AAAAAAAAh sweet revenge!!!!!!!
Imagine you guys have cut up his nerves or you have experimented with him with some fancy unheard of surgery and the patient bleeds to death on your surgery table, or dies of anesthesia and you want us to save your ass, and you want us to talk it out with the patient and we refuse to do so. Wow what a blast!!!!!!
That's gonna be fun baby!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
I'm loving it!!!!!!!!!!!!!!!!!!!!1
Paul
9/3/2008
"Dr". SDJ - seriously?
mainoralsurgeryman - you're preaching to the choir (and i'm a gp)
Dr SDJ
12/24/2008
Well a reputed endodontist of world renown on visit to India who came to teach us how you can avoid endodontic instrument separation broke his endo instrument while demonstrating on an extracted tooth! Funnier still he didn't even realize what had happened. It's only when the audience giggles went out of control did he stop his lecture to find out.
Sinus lifts are demonstrated on egg shells initially. Our world renowned demonstrator perforated each and every egg lining! Me and my partner elevated six egg shell linings each without a tear.That was our first ever attempt to elevate egg shell linings.
Goes to show that you specialist guys are mere mortals like all of us. You suffer from the same foibles we petty GPs suffer from.
Next time instead of looking down upon us GPs try a more help full exchange of views. Believe me life will be a musical harmony after that.
I am sure you will thank me for that.
About this I have no doubt!
MainOralSurgeryManIsAlose
1/28/2009
Hey, what's up? I hope you like getting all those referals on Friday at 4:30 for a failed atempt at an extraction of perio-compramized #8 from the unsufisticated GP classmate whom you cheerfully send baskets of cookies and cheap wine to during the holidays.
There is a mounting force of highly educated and experienced GPs who not only have surgical, pharmacalogic, and anaesthesia knowledge; but in addition we have prosthetic and restorative skills and knowledge that you will never have the will to learn. Furthermore we have people skills, we can out treatment plan and educate our patients better than any OMS.
So anyhow the cats out of the bag, its on the downswing for you guys so I hope you have hospital privalages and trauma skills, because I garauntee not only will your implant referals taper off to nothing but the rest of your rereferals will deminish by 7-10% per year. Why???, because of the attitude of the community of OMS exemplified by "MainOralSurgeryMan".
I defy any OMS to dispute this opinion and inevitable occurance.
R. Hughes
1/28/2009
I agree, there are specialist that have their panties in a wad because they believe they are entitled to referrals. They have to earn the trust and appreciate the business. I am a gp, yet very well trained and educated in implant dentistry. Because of this, I do not feel the love from some specialist, but others are comfortable with the issue. They are all talented, yet some are childish.
sergio
1/29/2009
I think Mainoralsurgeryman meant well. maybe it shouldn't have come out that directly? but I see his point.
What I like to say is that nowadays everyone is generalizing everyone else. Some one has a lot faster learning curve on certain topics than others and some others, after they pick it up, they advance very fast. And yes, there are those who lack the knowledge and skill unfortunately. Im a gp but I was in gpr that was very heavily focused on surgery and internal medicine. I take care of all the surgical cases in the office without any referrals. then again, there were other residents who still can't take out #8 in a broad daylight even after a few years of the training. So please, let's be supportive to each other and remember when we started doing the procedures for the first time. we weren't experts from a get go either and even now I come up with questions now and then about simplest things. If specialists have more knowledge than gps just for the amount of training they had, what about the years of gps spent on their pracices while specialists were on their additional residencies? Isn't that considered training?
Dutchy
2/2/2009
To MainOralsurgeryman,
I am a stupid GP placing implants, but I try to refer the more difficult cases to my oral surgeon in my place. Well since you know everything maybe you can give me some advise in the next case. The oral surgeon placed a implant in the region 3.6 (left molar lower yaw) and 8 weeks later the prosthodontist working with this oral surgeon placed the crown. I refered the case because I thought some vertical bone augmentation was needed in this area and I found it to difficult to do so. After 8 weeks the patient comes to my practice with dark colloration of the gum and bleeding when brushing this area. When I took a x-ray allready two treats of the implant was placed above the bone ( not caused by resorption). The gum I have been able to stabilized it by using a diodlaser and no bleeding occurs anymore and the gum looks sound, There is only discolloration because of the implant and abutment shining through the gum. Should I graft this place to get a better prognosis in the future? To whom do I refer to , because the oral surgeon doesn't think this is wrong? It is not my standard of care to put in a implant like this just for the money. I would take the risk and try to augment first although I have to take some risk of failure in the start of the procedure and maybe loosing the patient after failure of this procedure then having a late failure by putting in an implant with allready two treats exposed above the bone, just because it is faster and easier. So what should we do when the specialist in failing and refusses to refer?
Bill Schaeffer
2/2/2009
Dear Dr R,
You have started a most stimulating thread!
Can you tell us how things are with this patient now?
Kind regards,
Bill Schaeffer
Dr SDJ
2/6/2009
Last month the first patient ever whom I referred to an Oral Surgeon who is an implantologist came back with a broken crown, The crown was also restored by him! Since the implantologist has a string of degrees how should I counsel my patient?
MainOralSurgeryman since you know everything about OralSurgery and implantology please tell us.
And I am not being sarcastic.
dr sheida
7/29/2009
why exposed implant is harmful?
even small exposed area?
prof.Dr.Hossam Barghash
8/3/2009
small exposure is more harmfull than a big one, cos it well be difficult to clean the area.if u confronted with exposed implant,Never attemp resuturing, the best is to connect the fixture with gingival formar& leave the gum to heal .with good oral hygien.
Dr. Ares
4/9/2010
Dear Dr R,
I have some questions regarding your case. Why did you decide to place the implant 2 weeks postoperatively and not immediately? Was there infection on the tooth extracted? Was the extraction difficult, or was it atraumatic?
Suturing or operating on recently traumatized tissues, as I have learned the hard way, sometimes isn't the best choice. You decided not to suture the second time around, and I think that shows you learned that lesson too.
If only the cover screw was exposed, that shouldn't be a problem given the patient has very good hygiene. Usually prescribing a rinse with clorhexidine gluconate 0.12% is enough to control any bacteria around the healing wound (similar to immediate implants without a flap closure).
I would worry more about the throbbing pain still after all the antibiotics you prescribed. It seems that you were suspecting an infection, and a complicated one I must say.
Does the site still have any signs or symptoms of infection?
Pain is definitely a sign you must not ignore. If it is indeed infected, consider removing the implant and grafting the site.
I hope it all goes well with your patient.
And to the other bloggers, I am shocked at many of the comments made in this post. I think treating others with respect is fundamental. I am an Oral Surgeon, and would never treat a GP as an ignorant because he or she refers a case. I believe everyone here is reading these blogs to learn from each other's failures. I am very grateful we can share experiences and learn from each other.