XIVE Implant Bone Loss Case: Options?
Dr. C. asks:
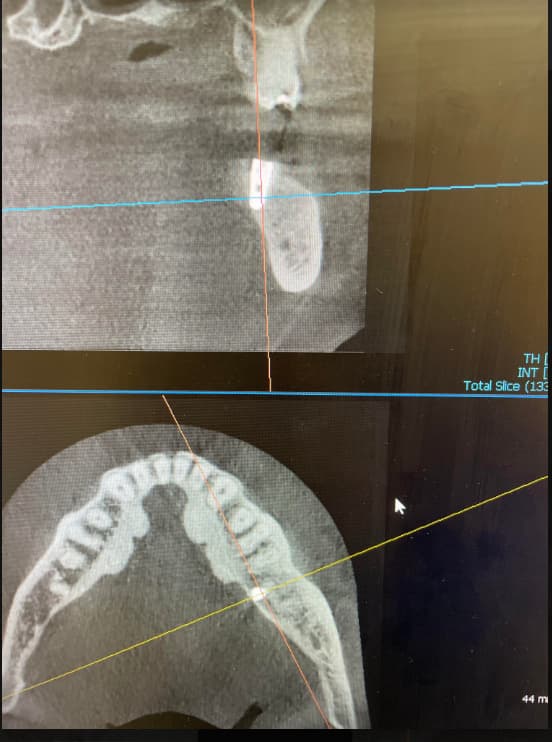
I am a prosthdontist. I recently placed a XIVE [Dentsply] 4.5mm x 13mm endosteal implant in the region of #19 [the mandibular left first molar; 36] in a healthy female patient. The installation of the implant fixture was uneventful and the healing was unremarkable. The patient returned for the uncover [Stage II surgery] 9 months later. Uncovery was unremarkable and I placed a gingival former. Radiography revealed significant bone loss around the implant fixture. What could have caused this drastic loss of bone around the implant fixture? What should I do next? What are my treatment options?
PRE OPERATIVE OPG
DURING OSTEOTOMY
AFTER PLACEMENT OF IMPLANT
AFTER PLACING GINGIVAL FORMER
LATEST OPG
15 Comments on XIVE Implant Bone Loss Case: Options?
New comments are currently closed for this post.
Dr. C
5/9/2011
When did you first notice this? Did you not follow up the patient before then? If the patient had a partially exposed cover screw for nine months that can create some infection. I usually see my patients s 2 weeks post-op and 6 weeks post-op.
sb oms
5/9/2011
This is not a cover screw infection. This could be from one or a combination of the following
1. Massive bone necrosis as a result of heat or pressure (compression) generated form surgery.
2. Surgical infection - contaminated implant site (either from residual bacteria or surgical contamination)
3. A ridge that was too narrow with a buccal or lingual dehiscence during surgery.
In my hands, the follwoing would make sense:
1. Removal of implant with graft - confirm dimesions of residual ridge
2. 4-6 months healing time before re-doing
3. Pre op scan- this is now a complicated case and the stakes are a bit higher.
I would not try to salvage this case. Just be honest with your patient, tell them that they have had a less than ideal outcome and that you don't want to put a tooth on an ailing implant. I have never had trouble when I have used this approach.
Thank G-D this doesn't happen very often.
Dr C
5/9/2011
I still think we need to know when he last saw the patient. Most of the possible events listed would be evident at 6 week period. Do you place the implant and then not see the patient again for 9 months? I will get the occasional patient that does not return for follow up. This would play a role in the handling of the case. If the patient had return for routine follow up care you might have been able to identify this earlier and the outcome could have been quite a bit different than the case your facing. My point being, If I would have run into a situation like this early in the healing process I am more willing to replace implant at no charge or discount. But what you have got now will become more involved and much more time consuming to repair.
Dr. Amer A. Jasim
5/10/2011
My advise you can measure the stability by stability analying devise and if the reading more than 50, I think better to reopening the site: do curation, good irregation and augmentatin by bone graft and make sure the bone completly coverd by mucoperiosteum.
Dr W
5/10/2011
Sorry this happened - sux when it does. Fortunately as was said before, it doesn't happen often. I would agree completely that this may be an overheating/bone compression type problem. Bone looks to be dense on the radiographs. Otherwise something obscure like residual infection. This would be a serious dihiscence to see that kind of bone loss so for me, that might not be as high up on the list of possibilities.
Back it out, clean everything up, graft graft graft. Consider PRP or some autogenous bone - its a big defect. Scan it in 6 months and see what is there. Hopefully you'll get a second chance on it.
Best Regards
Pankaj Narkhede, DDS; MDS
5/10/2011
I don't see a rubber dam clamp - just kidding
Anyway-
Comments by sb oms are the ones that I will repeat. If this was a flapless surgery and a scan was not used you had no bone buccally after the implant was placed. Secondly, infection during healing.
If the implant has some osseointegration and is stable may be a titanium mesh with tenting screw will help. (kind of risky though). Explain the patient.
Ali Hossein Mesgarzadeh
5/10/2011
Dear Dr.C
As we can see in immediate post operative PA radiograph (coronal segment )microthreads of fixture are exposed so it may be a main cause of infection around the collar of implant.Anther important point that i can see in radiograph,there are some radioopaques foreign body around the collar of implant,what are these particles in mesial part of implant ?Are there bone substitutes ?! or just some radiographic artifacts? sharp alveolar ridge is another cause of bone resorption with small bacterial infection .I also agree with sb oms comments.
Don't worry it may happen for everyone in surgical practice.
Best regards
Dr. Ali Hossein Mesgarzadeh
DDS-OMFS-MS
Tabriz / Iran
Dr Sanjay Jamdade
5/11/2011
Dear Dr C sorry to see bone loss in your case.
The commonest reason to see bone loss of this pattern is due to pressure necrosis of the bone. Implants are tapered apically and cylinderical in the coronal half. The Apical tapered segment of the implant is well integrated and the coronal cylinderical part is the one without bone.
When the tapered implant goes into the osteotomy, resistance to torquing is noticed. This resistance often comes from the implant pushing against the cortical plates.
The crestal/cortical drill is designed to relieve pressure off the cortex. If the cortical drill is not used when one torques the implant, the cortical plate gets tremendously pressurized and the bone may either fracture or get necrosed.
If the resistance to drill has been encountered thread formers (bone taps) should be used.
Another way to cause pressure necrosis is by skipping drills or not taking drills to length. Often osteotomies aren't cyliderical axialy but rather get a little curved due to wrong wrist movements. This can produce resistance to placement. Hence it is recommended that trial implants be placed to see if implants of desired width would got to desired length.
Heat generation and heat related necrosis is also a possibility. Even if you torque in an implant too fast with a hand ratchet you can generate heat.
About infection getting into the osteotomy site- one probability is through using internally irrigated drills which have the 'shmuck' from the previous patient. Internally irrigated drills have to be cleaned with a needle supplied with the kit and then irrigated with hypochlorite and washed thoroughly. You will be surprised with the amount of stuff that comes out of the drills. This clogging is often related with low saline drip speed in the previous patient. Also for the patient on hand, foreign proteins are transfered and the drill gets only external irrigation if any. You get heat and infection related bone loss this way.
If the incision gets botched up and the periosteum gets damaged while raising the flap, you could have a crestal bone loss though not as much as this case.
Other mundane possibiities like choosing a wider implant than permissible, patient having calcium metabolism issues, patient giving history of smoking or consuming bisphosphonates(alendronic acid) for osteopenia could be evalauted.
By the way you seem to be an experienced implant user anyway, the paralleling pin used is not from the Xive kit and is probably from a Frialit 2 kit (?). Unless ofcourse if the company changed the design! I think you should be able to figure out for yourself.
Dr.Sridhar Chowdary MDS
5/12/2011
Thank you very much to all of you for your responses.These are very useful.I will keep updating you about this clinical case.Thanks once again.Dr.Katta sridhar Chowdary M.D.S.
ttmillerjr
5/14/2011
Sounds like the issues have been addressed, but here's my two cents; I think a partially exposed healing cap can cause this type of infection. Just like a wisdom tooth that isn't fully erupted, the patient can't clean it. I can't see the exposure of microthreads, but if they were exposed this could have added another risk factor.
Kor
5/17/2011
I agree with all the post above....from x-ray it could be plaque getting around healing/cover screw or overheated bone.
On another note, I am not too crazy about Dr. C's comments. It is great to see patients soon after implant placement BUT--peri-implantitis can occur at any stage. If you are lucky enough to catch it early that is great, but to say that two week interval or month interval would have seen this, not always true.
Also, regardless if patient showed up for post op or not, this case should be corrected an no charge to the patient. Reason being is, law suits are very easy to file. Can you guarantee that the reason for this failure was not the result of the operator? I have placed over 1000 implants so far and have had to replace 3 of them so far. All of them at no cost to the patient and one of them even an additional implant placed.
Unless the patient is being so unreasonable that you would take your chances going to court, the aggravation and stress is not worth a few hundred dollars to redo one. Just my two cents.
Dr. Both
5/21/2011
I think the reason why the implant lost so fast so much bone is because of the high gingival former who is in okklusion. The patient could bite on it.So here we have bone loss because of immediate loading. In that case i would explant it and graft.The chance of gaining some bone is 50-50. The periodonatl attachment by the adjacent teeth ist still ok.
Abg
6/10/2011
Dear Dr
severe bone loss cud b due to periimplantitis. given the information that the patient reported after 9 months with no routine follow ups(maintenance regimen). Implant is integrated at the apex with loss of bone at the coronal( cud b indicative of periimplant infection???).This is just an hypothesis, bcoz if the reason is heat necrosis then how is the implant stable at the base(bone loss not encompassing the entire body of implant,which wud have been seen if it were to be heat necrosis). No evidence based or literature based support only hypothesis.. Experts please comment..
LB
6/17/2011
I need your help here.
Some of you guys say 'partially exposed healing cap can cause this type of infection'. What about when you do an immediate loading? Is the implant not exposed to the oral environment/bacteria/plaque? Am I the only ignorant who given the right circumstances place a healing cap straight away?
P.S. I am honestly not being sarcastic.
Dr. Omar Olalde
8/15/2011
I totally agree with LB, I really don't think is an infection caused by bacteria around the healing screw,and what about the "one stage surgery" when you place the second fase healing screw when you place the implant; or what about the one piece implants or the immediate loading. In all these cases the gingival tissue seals on the implant neck.
You can confirm if you have an infection doing a blood biometry, and the results of the leucocites is going to determine that. In case of infection of course is an anaerobic infection, that can be treated with metronidazole.
It could be a lot of pressure on the neck? Yes but you would lose just one third of bone not two thirds.
If the implant is stabilized with no infection I would regenerate with particulated graft and a titanium mesh with a PTFE membrane or PTFE membrane reinforced with titanium.
Right now I'm having a 54year old patient with the same problem in anterior maxillae but she already have lost the two implants and there is no bone, this after one year of LOADED. There is no infection, all blood tests OK, but lost all the bone palatal, labial.
An Endocrinologist gave me his point of view abour Vitamin D.
I'll write if I have more information.
Good luck.