Ailing Dental Implants and Infection: Causes and Treatment?
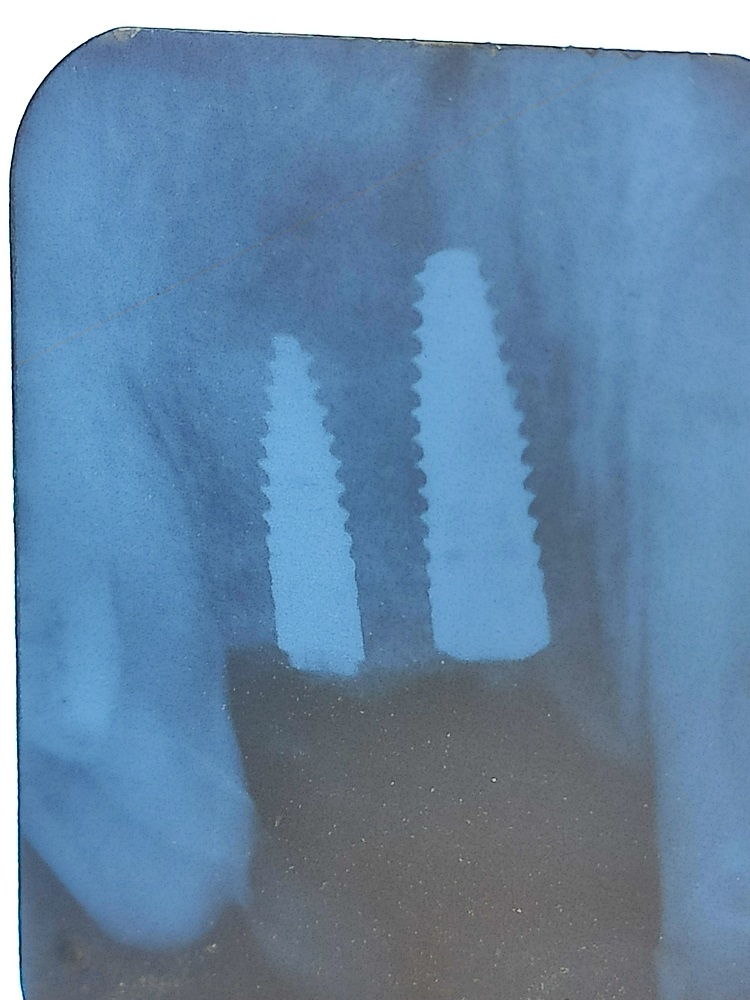
Xray for this case is at the bottom of this post.
I am a Male patient, 25 year old and in healthy overall condition. I had an extraction of the central and lateral upper incisors due to trauma on the central many years back and then infection of the apex which was treated by root canal, which subsequently failed. A fistula arised and while the tooth was treated and filled with calcium compound (might be calcium hydroxide, but I can't remember). Eventually the area kept getting infected, which also damaged the lateral, so both were extracted.
There was moderate/severe bone loss due to recurrent infections so Bovine bone graft was put in place at the same time as extraction and the site healed uneventfully for 10 months. 6 weeks ago, I had dental implant surgery for both central and incisor, placing two Straussman dental implants in the regenerated area. Also the dentist added some more bone graft to "fill in" some remaining defects, and a gum graft was performed to cover everything up.
I was put on antibiotics (amoxicillin 500 mg, 3 times a day for 7 days) and healing seemed uneventful.
After 2 weeks of placement, sutures were removed and everything looked fine. 4 days afterwards, an abscess formed around the gums where the implants were placed. the dentist drained the pus through an incision and put me on a course of antibiotics, (amoxicillin + clavulanic acid, 3 times a day for 2 weeks) to see if the infection might be due to suture removal. Although the antibiotics reduced the infection, some "tension" was still on my upper gum close to the nose area, and whie pressuring, the dentist found a tiny bit of pus, and decided to open up 4 days later.
Upon opening (week 6 after dental implants placement), the dentist mentioned that the bone graft seemed to be healing uneventfully and that signs of the source of the infection were not visible. The implants were stable. The dentist debrided the bone graft (taking out minor granulate tissue she found, according to her own words) and applied local tetracycline to the area. antibiotics were continued throughout and ordered for 10 days after operation.
Now I'm 6 days after this intervention and I feel there is again swellness in the area, which feels like some liquid, so I'm assuming the infection is back.The dentist said the CT Scan didn't show any problems or bone loss. The adjacent teeth were checked for vitality and gave positive, which alongside the CT scan discarded endodontical problems in them. I have attached an X-ray from 4 weeks post-op.
What could be the source of the recurring infection? How would you proceed? It's the aesthetic zone and I took a lot of time to let everything heal in order to do the implants right and they still failed. I'm also worried because between these failed saving attempts, I've been on antibiotic treatment for almost 4 weeks non stop, which sounds way too much from my persoective and with possible new infection, probably more rounds will be needed.