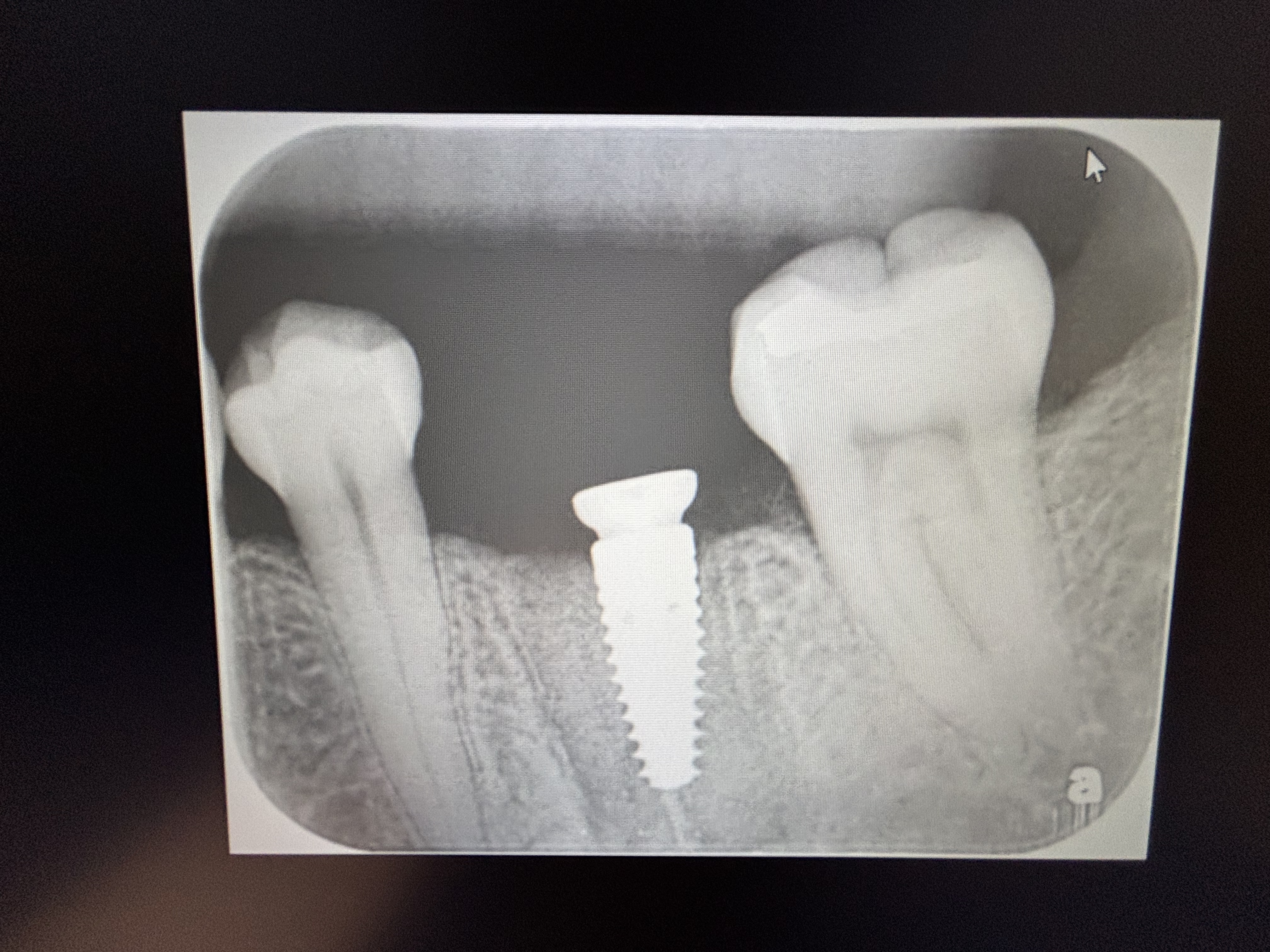
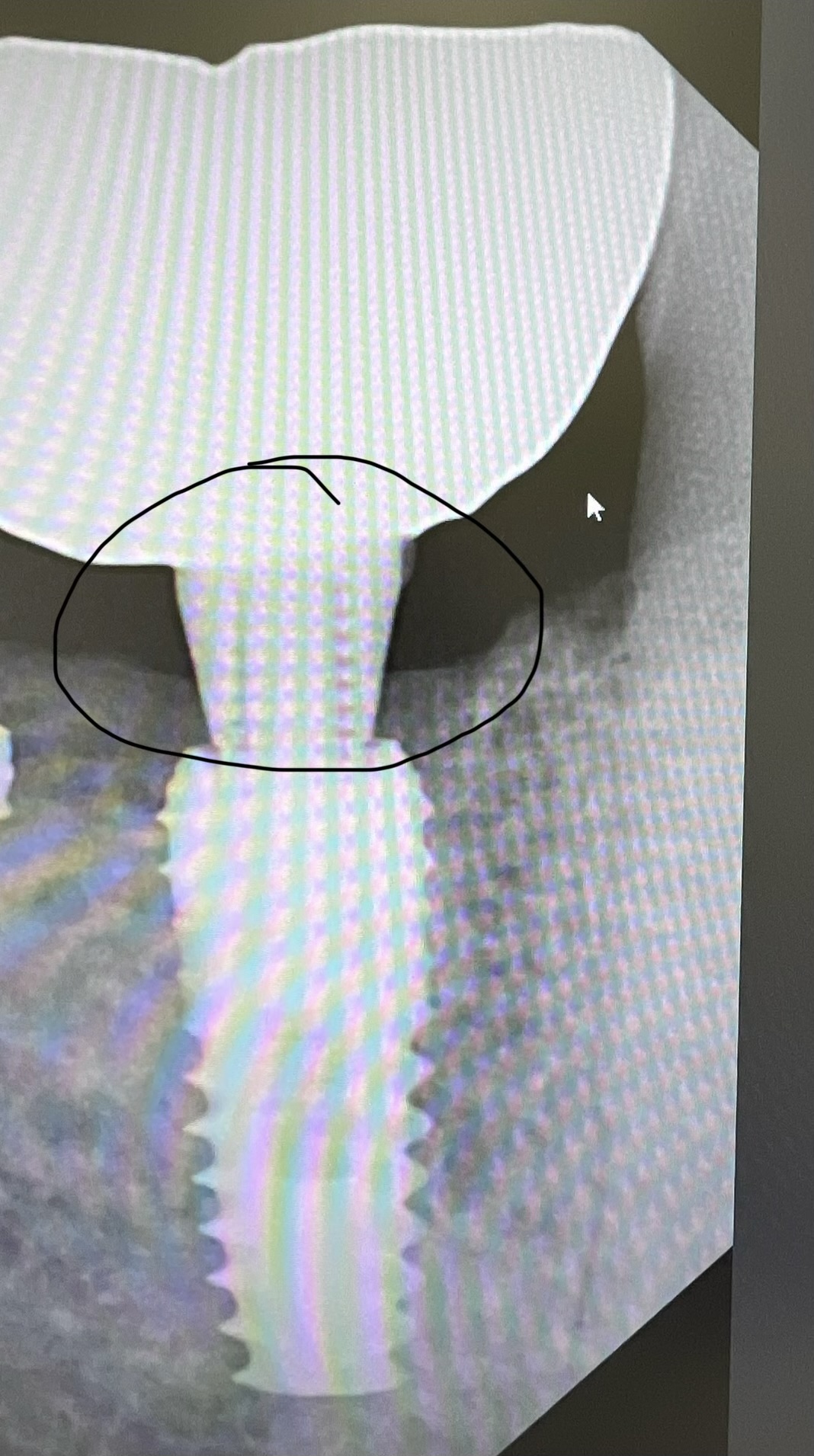
Apical Fenestration: Recommendations for Treatment?
Dr. O. asks:
Patient presented with a recently placed implant fixture with a fenestration in the buccal cortical plate at the level of the apical third. The implant has osseointegrated and has primary stability. What procedure do you recommend to treat the fenestration? What kind of bone graft material do you recommend? What chance of success should I expect from this rescue treatment?
24 Comments on Apical Fenestration: Recommendations for Treatment?
New comments are currently closed for this post.
John Kong, DDS
2/27/2012
GBR. Sandwich technique - Autogenous bone (osteoinductive bone) next to the implant with Cortical Bone (slower resporption hence space maintenance) as outer later covered by membrane and tension free primary closure.
OMS resident
2/28/2012
I just wonder, why are you planning on treating the apical fenestration when the implant has osseointegrated?
By the way, "primary stability" is a term used at the time of implant placement, not after the implant has healed and integrated.
Kong: What kind of "Cortical Bone" are you talking about? Auto-/allo- or xenografts?
John Kong, DDS
2/28/2012
I like Puros Cortical and the only time I use Xenografts is for sinuslifts because that how I was taught and I'm even moving away from that. I basically think Xenografts are garbage.
Drb
2/28/2012
Is there an active infection? How old is the patient? Which tooth # is it replacing? I've had good success treating these after disinfecting with chlorohexidene soln, by creating a few tiny bleeding points in the bone adjacent to the implant. Then using Dembone and a resorbing membrane. If you cant get the membrane stable use screws. I suture with PTFE as the wick the least. Evenso I cover the site with Atrisorb if the patient can tolerate tetracycline.
gary weider
2/28/2012
X-rays/photos would be nice so at least we can guess what the etiology is. How long has the implant been placed? What's the perio condition? Assuming everything else is appears healthy, I have had a similiar situation which I treated this with Augmentin and it eventually went away.
Richard Hughes, DDS, FAAI
2/28/2012
Dr Kong at least you and I agree about xenografts. They can be worse than garbage.
peter fairbairn
2/29/2012
Guess this was another "flapless" case , agree a bit confused about osseo-integrated with good primary stability ........ but guess it was placed a while ago and when coming to load the fenestration was noted.
Here raise a site specific flap , do not raise a full flap , LEAVE the crestal attached gingiva if there is bone at that area . Then clean the implant surface and graft with a synthetic that is full bio-absorbed and sets to be its own membrane . Then you will know tou have bone and not merely HA and fibrous tissue when the body has regenerated the area .
Peter
Baker vinci
2/29/2012
Are we gonna start grafting apically fenestrated, asymtomatic teeth as well?? Bv
Baker vinci
2/29/2012
Placing cortical bone at an apical fenestration, is the wrong answer. I don't care what kind of bone it is. I would have made this response, regardless of who suggested it. In order to place a cortical strut, it has to be rigidly fixated. You talk about turning people into patients ! Leave this person alone, please. Bv
Baker vinci
2/29/2012
Peter, if you raise the flap in that way, aren't you closing the wound directly over the graft. I might be misunderstanding your description. Respectfully bv
John Kong, DDS
2/29/2012
Have you taken out an asymptomatic impacted wisdom tooth? Then, stop being so melodramatic when it's doesn't need to be.
Baker vinci
2/29/2012
No kong, unless it has a perio pocket with exudate, or if it looks likes it's going to error the second molar . I talk a lot if people out of third molar extractions , in that there is no literature to proove they move teeth. Bv
sergio
2/29/2012
I'm with BV on this one.
The implant is solid because it's osteointegrated.
Some 40 -50 % of anterior teeth have fenestration. According to research done by Italians, not all of the fenestartion is developmental.
So, you are going to put graft there as well?
Let's not treat a problem that's not there unless there's active inflammatory process going on consuming bone around the implant.
Baker vinci
2/29/2012
What omfs program did you attend? Bv
JIM
3/8/2012
What does that have to do with anything?
Baker vinci
3/8/2012
Well Jim , it has a lot to do with this particular case. I am being told to stick to wisdom teeth and let the experts deal with the "BRONJ". I'm my part of the world we are "the experts", when it comes to this condition and others like it; such as ORN, osteomylitis , pathologic fractures , carcinomas and neoplasms of the maxillofacial region and if his program did not instill this philosophy in him, then his credibility has to be questioned. He makes some pretty damning and emphatic statements, again, patients are looking to this site for help, just as I am trying to augment my knowledge, by learning from others . Bv
peter fairbairn
2/29/2012
I totally agree on the wisdom issue BV , and yes Sergio a suorising number of our "sucessful " Implants may have very thin bone buccally ( or even a fenetration ) so yes no worry just monitor.
But here as usual there is limited , slightly confused information given but there must be a bigger issue as to be noticed , be it a suppuration , a soft tissue opening or merely the meatl colour of the implant showing through ( Blueing ).
Hence why there is a desire to treat .
As to the site specific flap , yes BV it is over the graft site but using the newer graft materials that set allows this to be done safely and raising a full flap may affect the aesthetics.
In fact just done in the last hour a big Peri-implantitis case ( refered in ) but needed to raise a full flap to clean effectively .
Regards
Peter
jg
2/29/2012
Im stiil confused...from the original question....is the fenestration sub gingivally...not exposed to the oral cavity, if so how can you tell..? if exposed to the oral environtment.....???? whats the question you all make a big scandal if a couple of threads are left above the bone level when placing...why???? THATS RIGHT....!!!! It holds bacteria!!!...My opinion, if that perf happened at the time of surgery it should of been grafted then!!!..If is coverd, by tissue, and not creating and esthic problem,I would leave alone..How many times do oral surgeons, go through both mandibular plates and protrude implants inferiorly, with no consequences......
John Kong, DDS
2/29/2012
Baker, sometimes I wonder if I'm being punked by your responses and comments or even if you're really an os.
Regarding wisdom teeth, the 'white paper' which your specialty organization released states on page 4:
"AAOMS fully supports the elective, therapeutic removal of impacted
third molar teeth that are not likely to erupt into a disease free position, whether the third molar teeth exhibit symptoms or not, and preferably prior to the onset of periodontal or pericoronal disease."
So basically, they support the removal of asymptomatic 3rd molars IF there's a 'possibility' of it causing "problems" in the future.
A fenestration defect on an implant (apical 1/3) is COMPLETELY different from a fenestration defect on a natual tooth. The root of a natural tooth as cementum and PDL along with the protective mechanisms that come with that whereas a dental implant does not.
If you want to leave the fenestration alone b/c its covered by the mucosa, fine, but if you want to treat it b/c of the 'possibility' of it causing "problems" in the future or there's exposure of the implant thread, that's perfectly fine as well.
All I know is a fenestrated implant is not what I aim for when I place an implant and if there is one, I want it cover it with bone (99% of time unless it will do more harm). In your practice you may not care if your implants are fenestrated, but in mine I want better for my patients.
Baker vinci
2/29/2012
Dr. O, is the implant fenestrated at the bony level, or is it dehisced through the mucosa. If you are seeing the fenestration on ct exam, only, then I would leave it alone. If you have a mucosal dehiscence, then the correction of this, is pretty challenging. Just as most experienced posters have mentioned, I would not fret about the lack of apical/ buccal bone, especially if you have good mucosal coverage, good integration and no disease at the region of emergence . The way I understand it, more than 300 degrees of the implant is surrounded with bone. You may very well create a mucosal exposure, if you choose to proceed. There are no real "parameters of care", with this scenario, as you present it. Let your patient get a second opinion, from someone you know, doesn't" cut for the sake of cutting". Bv
Richard Hughes, DDS, FAAI
2/29/2012
Baker, it is recommended to treat a fenistrated implant. They are not teeth. How to treat ( graft material, membrane, flap design) are the issues. I think Kong is a perio, I could be wrong.
Richard Hughes, DDS, FAAI
2/29/2012
Baker, I retract my last statement. If the CT shows
Major bone support observe and tx later if needed.
Baker vinci
3/1/2012
One more, Ill advised response to you, kong. I donated a large sum of money, to support the science that was required to keep those residents fed, for the hard work, that went into the "white paper" and it is a sound study. In the adult population, anyone over 24-27; I have to have a legitimate reason to operate on them, for whatever reason. If the teeth or fully covered with bone and completely apexified, they usually stay . My apologies to the other posters, for the redundancy and uneven "piss match", that I let myself, get into. Our "association ", also encourages orthognathic surgery, for the 1-2 mm open bite, or the 1-2 mm micrognathic lower jaw. I reserve this type of surgery, for true deformities. These "things" are guidelines, by which we choose to practice. I am aggressive with cancer/tumors and infections, only. The best surgeons in the world, are the ones that know when and when not to operate. Now, no more Yankee my wankee!!! Bv
dmitri
7/25/2012
Dear colleagues
What is your opinion,to cover dehiscense and fenestration,with autobone only(chips of cancellous bone) without using membrane
Thanks