Crestal Bone Loss: Can it be repaired?
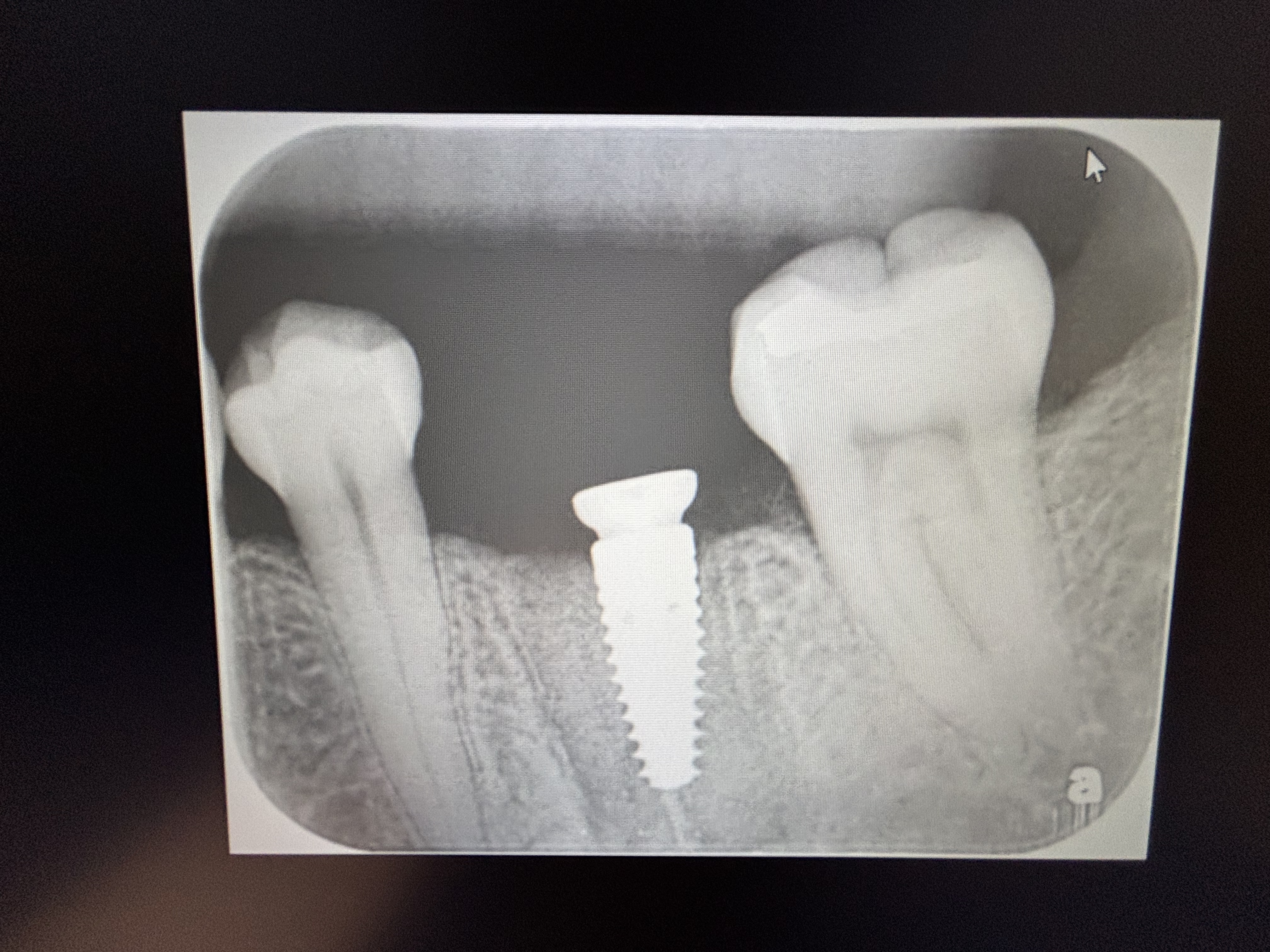
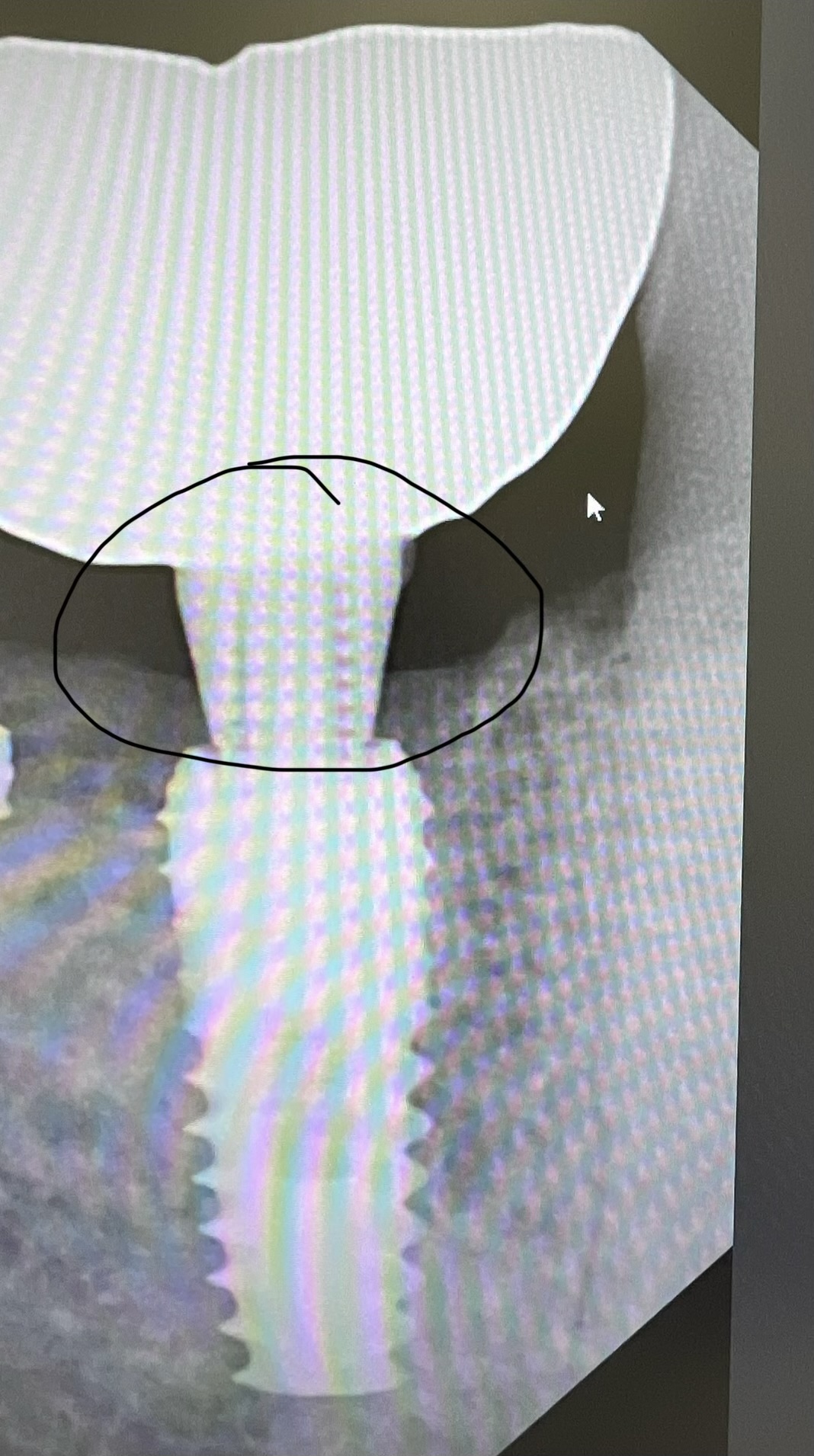
Implants (MIS 3.75×11.5 and 4.2×10) were placed without incident and with good initial stability on 5/19/2015. Implants drills used per MIS drill sequence including the final drill. Post-op at two weeks and two sutures were missing and the incision had opened. Irrigated with Chlorhexidine, changed the cover screw to a healing cap on 19 and re-sutured. On 9/29/15 patient came in for follow up and the second PA was obtained. 2 mm of crestal bone loss has occurred. Implants are stable. Can we place a titanium mesh and a graft and expect that to heal? Should we remove the implants? The patient is interested in restoring them as they are.

10 Comments on Crestal Bone Loss: Can it be repaired?
New comments are currently closed for this post.
CRS
10/2/2015
You are overtreating this, slow done let the implants integrate, place a ct graft in about six weeks if stable.Re suturing a flap at two weeks is a no no. Figure out why the crestal bone was lost, overheating, trauma, too much torque, implants placed too deep biological width violation. If you can't tell me what may have happened then it is difficult for me to advise you how to fix it. I am unfamiliar with the Mis implant if that is a polished collar then bone doesn't adhere to it. Titanium is overkill. The X-ray doesn't look that bad how does the soft tissue look and is the exposure progressing?
CAM
10/6/2015
The soft tissue around the implants look perfect and has healed nicely with adequate keratinized tissue at the collar of each implant. Placement was without incident. The MIS system has a final drill that it tapered like the implant and is recommended in Type 1 and 2 bone. The collar is not polished on the MIS implant. The MIS Seven implant "features" microrings on the collar. Other than crestal bone loss the implant looks perfect. The exposure is not progressing at all.
Don Callan
10/6/2015
CRS is 100% correct!!!
Tony Collins AM
10/6/2015
2 reasons that flaps open - knots not properly tied or flap under tension and sutures pull through. Buy a book on suturing (eg Silberstein). When you see movies of brilliant surgeons performing amazing surgery, then leaving the suturing to the junior resident, don't think that applies in the mouth - good intraoral wound closure is one of the most important (and demanding) aspects of oral surgery. Learn and practise different sutures - especially horizontal mattress. A leg of lamb is a good surrogate to practise on.
Misch (Contemporary Implant Dentistry Ed 3) discusses about 8 reasons for crestal bone loss around healing implants, and when questioned on this at a seminar, he replied that it is probably multifactorial. Some or all of the factors apply.
Personal experience has shown that in the absence of features such as gross occlusal overload or infection, crestal resorption usually stops at the first thread and is stable.
David Anson
10/6/2015
With the MIS-7, I find that if you place the top of the implant a little deeper, at the bone level (which is then about 0.25mm above the polished top of the implant, the bone stays very stable. You just have to make sure that the anatomic cover screw goes all the way down in the implant. Often you have to clear off some bone, which is easy with the "0" cover screw on the implant and using a round bur at 1500 RPM.
Brett Rabel
10/7/2015
I have had a problem similar to yours using an implant which is also similar. I use the AB I5 implant which is also a tapered implant. When I searched dental town to seek the source of my problem, I found that that type of bone loss seems to happen more often with tapered implants. My Final thoughts as to why it occurs in descending order includes: The tapered implant places pressure on the cortical bone and begins the bone loss(Maybe you placed it deeper then the final drill indicated) , I placed the implant below the bone level and placed the healing collar Which did not seat completely and caused the bone loss, The implant has a poor crestal design, I overheated the bone.
I have only been placing this new implant for around eight months, and I had no crestal bone loss problems whatsoever using a previous implant that was straight walled. I have not noticed this bone loss with two-stage surgery, only with one stage surgery with healing collar. It has happened more than once and concerns me as it does you. My situation is also similar in that the tissues are very healthy around the implants, so I have restored them all.
Has anyone else experienced this problem with MIs or AB I5 implant?
Sanjay anand
10/9/2015
Very useful discussion
Luiz Jesus
10/10/2015
Bone resorption crestal perimplantar occurs whenever or when the implant is exposed. It is a physiological reaction as research several authors (Turnow et al.) And is independent of implant screw architecture. Several factors can yes, increase loss such as Misch describes.
Personally I see no apparent reason to abort the prosthetic rehabilitation if the implant is stable
BigGoogootz
10/19/2015
Chlorhexidine: Good for soft tissue, bad for bone.
The depth of the bone loss is directly related to the depth of the penetration of the chlorhexidine.
Chlorhexidine is not a cure all. It certainly does not promote bone regeneration and is certainly not osseoinductive. Using it as an irrigation in the circumstance you described is like drawing your gun and shooting yourself in the foot. OUCH! The proteins on the implant combined with the chlorhexidine and formed a toxic coat on the implant and the bone said, "Oh, hell no" and left the building.
Nicholas Busuttil Dougall
6/14/2016
hi,
Interesting argument. Do you have any evidence to back it up? I personally use H2O2 post op as I read that CHX interferes with wound healing immediately post op. Maybe this is the same situation? Would apprecate your feedback. Thanks