Generalized Periodontitis: Treatment suggestions?
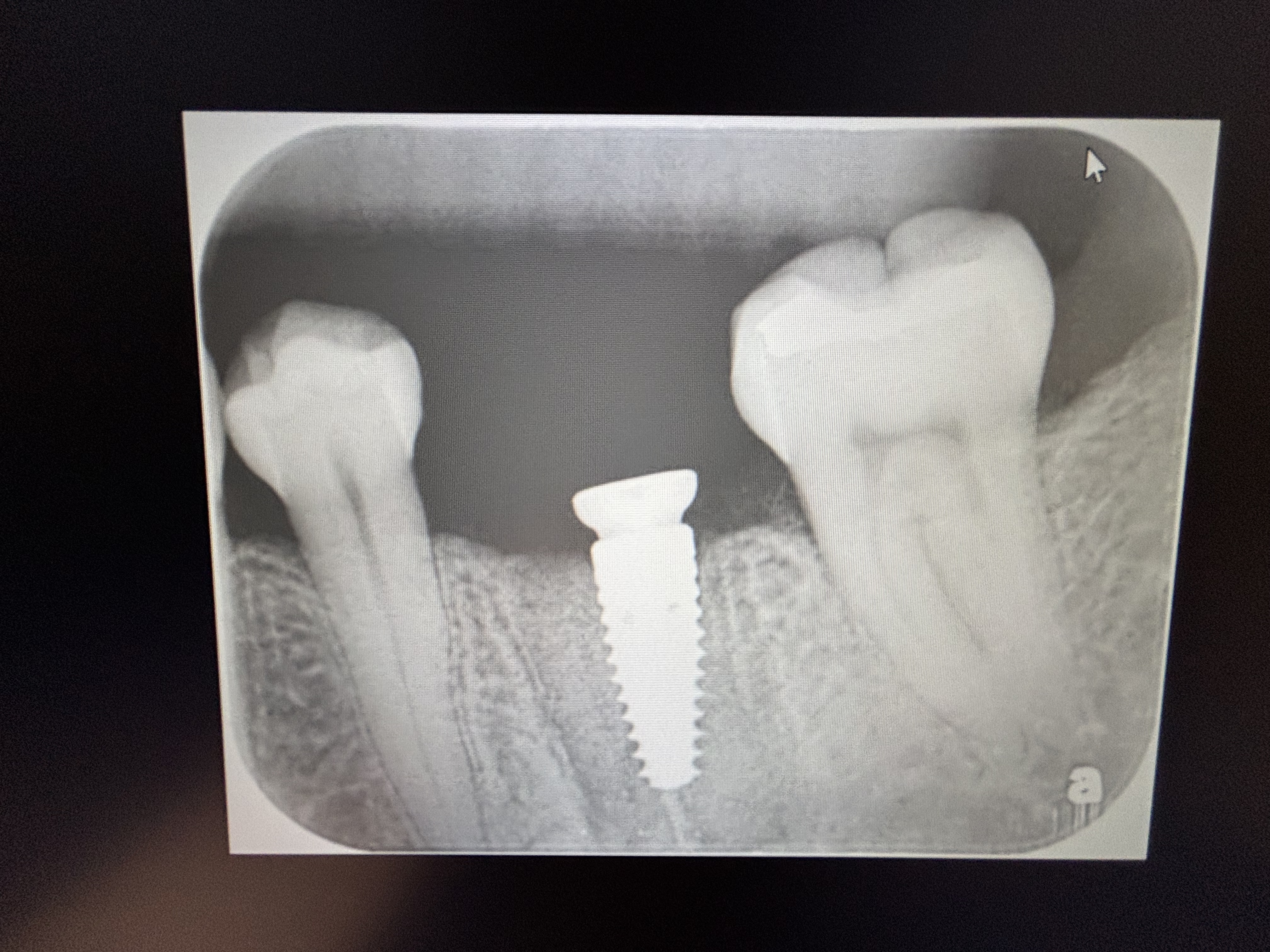
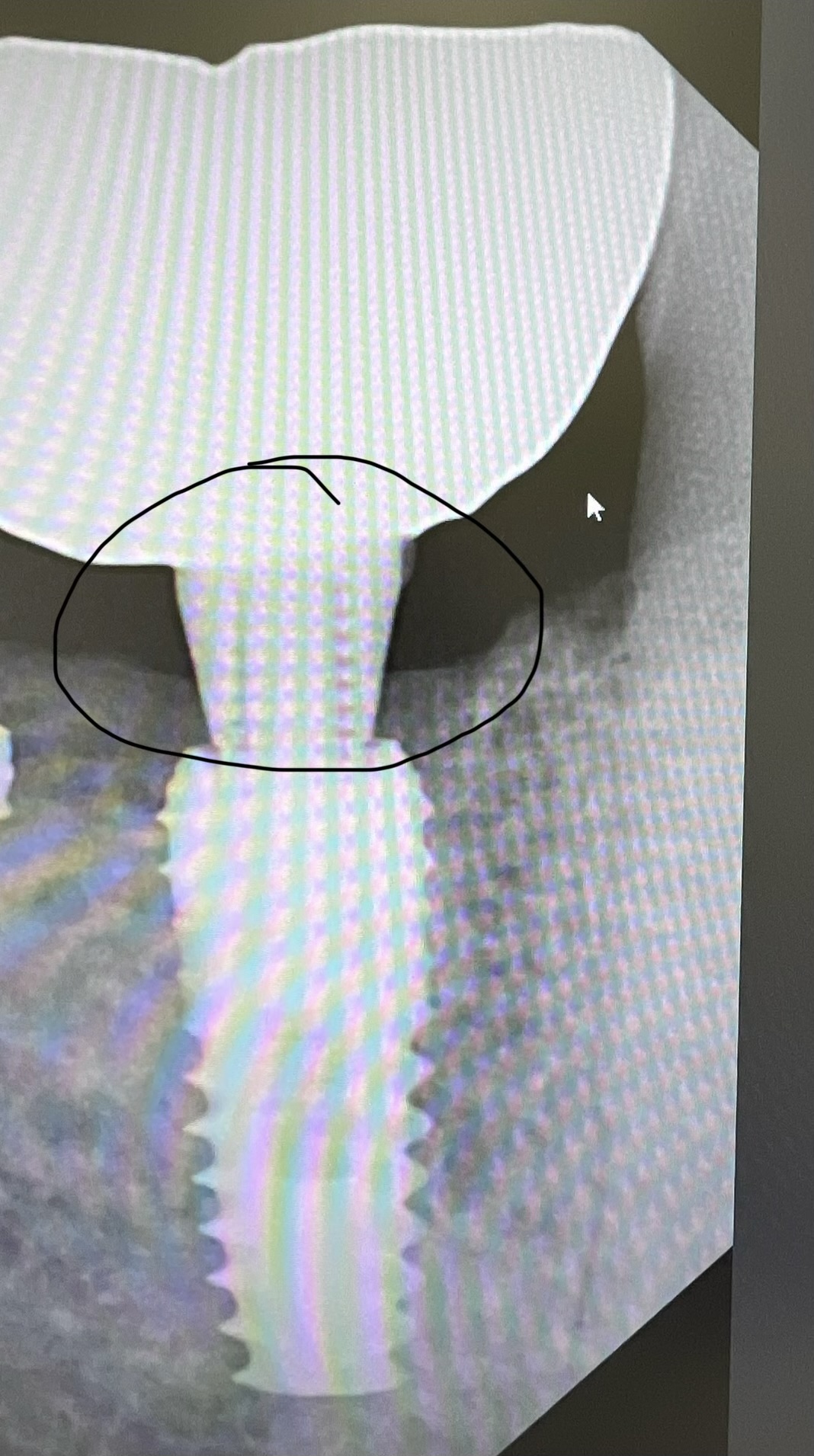
I have a 30 yr old female patient with generalized periodontitis. I did full mouth flap surgery with extraction of the rt. upper 1st premolar 1 month ago. Current mobility on the rt. upper first molar is grade 1. I am planning to extract the lower 2nd molar a little later. I am planning to extract the rt. upper 1st molar with subsequent delayed bone grafting and sinus lift followed by delayed implant placement after 6 months. I have doubts about placement of a bridge in the upper rt. Will this work? If so would you suggest going from canine to 1st molar or from lateral to 2nd molar? What would be the durability of a bridge there? A cast partial denture would be a last option given the age of the patient.













22 Comments on Generalized Periodontitis: Treatment suggestions?
New comments are currently closed for this post.
Dennis Flanagan DDS MSc
3/4/2019
This pt appears to have an IL-1 interleukin polymorphism. She may be best treated by a perio. At minimum 3month SRPs and systemic doxycycline may be in order.
Vipul Shukla
3/4/2019
As Dr. Flanagan said, this appears to be an adult periodontitis case with CAL, whether its a Refractory Periodontitis or just due to local factors and neglect is another diagnosis. A subantimicrobial dose of Doxycycline long term with scaling and root planing should help a lot.
I think a fixed four-unit bridge in Quadrant 1 is easier to do than 2 or 3 dental implants that you have proposed, don't you think?
Also, way cheaper and faster turnaround.
Research is showing refractory periodontitis cases are not good cases for dental implants either for long term success. The bridge may periodontally 'splint' the mobile molar while restoring function back. Reduce the pontic size if you wish to reduce the occlusal load.
Something to think about.
Thanks for sharing.
Peter Hunt
3/4/2019
As many of the teeth still seem to have good bone support, it may not fit in the generalized periodontitis category. It seems more a case of intensive, localized Rapidly Progressing Periodontitis.
This condition can be very difficult to treat. RPP can arise suddenly and progress very rapidly. This being the case it is probably not advisable to think of fixed restorative therapy as the natural teeth supporting the bridgework may get periodontally involved sooner or later.
The place to start is with intensive periodontal debridement, to attempt to stabilize the periodontal situation. She will need to be watched very carefully with fast interception if a new lesion starts up.
In terms of implant therapy on the maxillary right, an extraction + socket regeneration leading to implant placement may have the effect of losing considerable bone in the region, when there is not much there at present. With an immediate placement protocol it would be possible to expand the socket region, and to lift the sinus floor at the same time which generates additional bone volume for an implant as well as providing enhanced immediate stability in the sinus floor. Much the same approach could be used for the first premolar site (best to use it before it disappears) and maybe even the second premolar site.
This is a tough case that needs very skillful care to maintain the dentition oner the years, I hope very much that you can turn this case around. Best wishes!
Dr Dale Gerke, BDS, BScDe
3/4/2019
All comments are worth considering. The real issue is what is the aetiology?
I personally would not consider any form of restorative treatment initially until the periodontal problems are treated and stabilised. Until that time, any restorative treatment outcome would only be guesswork and likely not be in the best interests of the patient.
Even when the current problems are controlled (if that is possible) I think it would be unwise to place a large span bridge anywhere. There are simply too many unknown variables.
If bone loss can be arrested, then appropriate methods to regenerate bone and place implants could then be considered. Since absolute maintenance of implants would be critical, I would consider single unit implants for a multitude or reasons.
However with caution in mind, it might be prudent (after adequate periodontal treatment) to start with just one or two implants placements (in different quadrants – probably in the aesthetic regions) and review them for 1-2 years before embarking on full scale rehab.
As has been mentioned, this is a tricky case and it will require considerable skill and patience to have this lady retain her remaining dentition for a lifetime (or at least her posterior dentition).
As a small point, I would be interested in another radiographic view of the interproximal region between the lower left premolar and molar. I cannot make out what is going on but it might be something interesting.
Dr. Gerald Rudick
3/4/2019
Thus is a sad case..... a young patient to have so many periodontal issues....but what also must be considered is the spacing of the natural teeth, and the large multiple gaps that surely lead to food impaction. I think this patient has to be managed by an oral pathologist and a paeriodontis or someone who has good knowledge of how systemic conditions affect the oral cavity.
Elliot
3/4/2019
For the slightly mobile UR 1st molar try taking it out of occlusion totally. That may cure the mobility.
bigjulie
3/4/2019
Suggest daily use of a Waterpik with hot water and bicarb of soda. Effective, cheap and no contraindications.
Dok
3/4/2019
Gain full control of the perio problem before even considering any type of fixed tooth replacement. This patient should show perio remission for at least two years with impeccable home care and demonstrate a regular recall commitment. Give them removable pieces in the meantime. You are asking for trouble if you start placing implants and fixed work in a perio predisposed mouth coupled with poor homecare habits.
Don Rothenberg
3/4/2019
Is she a smoker? Sure looks it!
jerry schwartz,dds
3/4/2019
How was the patient's oral hygiene when she first presented...was there a large amount of supra and subgingival calculus...any chance that the patient is a borderline diabetic or a diagnosed diabetic...what is her glucose or HgA1C?
Suresh
3/4/2019
Thanks everyone for some really good thoughts.
Nope she's not a tobacco user at all.
Hba1c was 6
Done complete perio debridement.
Started doxy.
Will keep you posted regarding further poa.
Thanks again
Dr. Vishal
3/4/2019
As mentioned by other experts, all factors should be considered. If local deposits were not correlating with amount of destruction, thorough occlusal evaluation, specifically non functional cuspal relations should also be checked.
Andy
3/5/2019
I'm in the selective immunodeficiency camp here which doesn't necessarily preclude standard perio treatment of occlusal refinement, root debridement (I hate the term Scaling and Root Planing), curettage/JE removal flaps, bone grafting, implants, etc but requires immaculate control of pathogens going forward. I agree with delayed ridge augmentation until the patient gains documented control over pathogens. However I would institute general perio therapy right away beginning with debridement SPT and complete occlusal refinement with any parafunctional mitigation. See if mobility decreases and take it from there.
Randy
3/6/2019
Bottom line is that a periodontist should be a part of her treatment team.
Alex Zavyalov
3/10/2019
I would advise to unite all the teeth (both jaws) with a cast metal frame. It is functionally optimal and cosmetically unlike as in case of orthodontic brackets. It won't be as expensive as implant treatment and you will do no harm to the patient.
oralsurgeryjj
3/12/2019
Am I the only one who is thinking tongue thrusting habit?
Considering relatively intact left mandibular premolars with Spppppppppacious interdental area, I strongly suspect she has tongue thrusting habit.
And lack of proximal tooth support on isolated molars against medially vectored occlusal load had jacked up young lady's periodontum toooo easily. Right molar first, especially maxilla, which has relatively weak bone support, then left upper 1st molar next. That is my theory.
I would suggest checking her tongue thrusting habit on talking and swallowing, as well as tooth mark on tongue and size of tongue.
If my theory sounds plausible after examination, fix up her occlusion and tongue habit as priority or you probably be seeing her as your patient for the next two decades............... as complete denture patient at last.
Suresh
3/12/2019
Nope doc. Absolutely no tongue thrust habit
oralsurgeryjj
3/12/2019
Ha! hunch failed, anyhow I suggest ortho+perio first. That seems to be good "divide and rule" case. Isolated teeth will be on constant threat of peiodontitis.
Dr. David
3/12/2019
Refer to periodontist
DR.MAHIJEET SINGH PURI BD
3/17/2019
this seems to be a case of aggressive periodontitis.
treatment plan:
SRP
FULL MOUTH PERIODONTAL FLAP SURGERY WITH GTR PROCEDURE
ADULT ORTHODONTICS (TO RESTORE THE OCCLUSION) ESPECIALLY ON THE RIGHT SIDE.
FINALLY RESTORING THE SPACES ON THE RIGHT UPPER SIDE BY IMPLANTS WITH OR WITHOUT SFE (TO BE DECIDED LATER ON WHEN PERIO , ORTHO HAS BEEN DONE AND SPACES CLOSED AND OCLUSSION ESTABLISHED SO THAT THE CONTACTS ON THE CROWNS OF THE IMPLANTS AND OTHERS ARE ESTABLISHED.
follow up every 3 months with OPG for one year and then every 6 months in the second year and then once in every three years with OPG.
Bill McFatter
4/11/2019
does she have a hx of ortho? there is a possibility that the spacing is the result of a violation of the neutral zone from ortho attempts to close spaces. The original spacing could have been the result of the patient trying to breath. Post ortho could have resulted in a restricted space and now the patient is trying to re-establish space. The tongue is pressing the teeth in an effort to breath This is different than tongue thrust and the pressure can be laterally or labially. It looks like a diastema at 8/9 was corrected by the way 8/ 9 angles in and if straightened would fill that space at 9/10. This could be mostly iatrogenic with ortho ,home care, rapid movement and perio laid on top Is the midline centered ? Just a thought
Prof. Ana Pejcic DDS, MSc
4/12/2019
Dear Colleague,
I looked at the x-rays and read what you did and what you plan to do.
My advice to you is:
1. If a complete mouth flap surgery is performed, a minimum of 4-6 months must be carried out with regular controls to monitor how and to what degree the patient is motivated to maintain oral hygiene of the new condition of parodontium.
2. If she adhere to your instructions and on the controlled examinations, it turns out that the periodontal condition is satisfactory, you can think about further therapy.
3. The next big step in your treatment is the third molar in the upper jaw. It will certainly present you the problem at one time. It must be extracted if you want to do anything to help solve the problem in this region. In addition to the extraction of the third molar, simultaneous sinus-lift and insertion of the biomaterial can be done which will also fix the first upper right molar which is luxuriated. You should not extract this tooth because you will need it for prosthetic replacement.
4. After 6 months from the sinus-lift and the extraction of the upper right third molar, a fixed bridge can be made which will include the right upper canine, the first premolar, the first and the second molar as bridge carriers, and insert two members (the first and the second premolar).
5. As for the lower jaw, the second molar should not be extracted because it is in good condition. You will solve the occlusion by extracting second premolar (which is otherwise periodontal threatened by the extended periodontal space) and make a fixed prosthetic where the canine, the first premolar, the second and the third molar will be the bridge carriers, while the inserted members will be the second premolar and the first molar.
6. As far as the left side of the upper and lower dental strings is concerned, the insertion of biomaterials should be done for the purpose of preserving the teeth in the dental array.
7. Implants are not recommended, especially if hygiene of the oral cavity is not at a satisfactory level.
8. Also, all of the above implies a great responsibility of the patient and her awareness of maintaining adequate oral hygiene.
Sincerely,
Prof Ana Pejcic DDS, MSc, PhD
Periodontology and oral medicine
Specialist of Periodontology and oral medicine
Medical faculty, University of Nis
Serbia